JBRA Assist. Reprod. 2016;20 (3):112-117
ORIGINAL ARTICLE
doi: 10.5935/1518-0557.20160026
Socioeconomic profile of couples seeking the public healthcare system (SUS) for infertility treatment
1Centro
de Infertilidade e Medicina Fetal do Norte Fluminense / Departamento de
Medicina Reprodutiva do Hospital Escola Alvaro Alvim. Campos dos
Goytacazes/RJ, Brazil
2Faculdade de Medicina de Campos dos Goytacazes. Campos dos Goytacazes/RJ, Brazil
3Prefeitura Municipal de Campos dos Goytacazes. Campos dos Goytacazes/RJ, Brazil
CONFLICT OF INTERESTS
No conflict of interest have been declared.
ABSTRACT
Objective:
The number of couples seeking assisted reproduction services in pursuit
of the dream of conceiving a child is growing. In developing countries
10 to 15% of couples of childbearing age cannot bear a child by natural
means and the impossibility of conceiving a child has a significant
impact on the health and well-being of the couple. The aim of this
study was to evaluate the socioeconomic profile and the main causes of
infertility of couples seeking assisted reproduction treatment through
the public healthcare system.
Methods: We
analyzed 600 medical records of couples who sought infertility
treatment at the public healthcare system, and we divided them into
three groups according to age: 35 years, 35 to 39, and 40 years or
more. In each group we analyzed the cause of infertility, the number of
children of the spouses, the education level and family income.
Results:
The main cause of infertility was male-related in 34%, followed by
tubal factor in 31.5%. We found that 56% of the women were less than 35
years old and 58% of the couples earned less than 3 minimum wages.
Conclusion:
The profile of the couples was: low-income, low education and less than
35 years of age. The cost of assisted reproductive treatment is still
high, being restricted to couples of higher socioeconomic statuses. An
effective public healthcare policy could minimize this problem by
improving the quality of care for couples seeking infertility treatment
at the public healthcare system.
Keywords: Assisted human reproduction, Infertility, Socioeconomic status.
INTRODUCTION
With the spread of assisted human reproduction techniques throughout
the world, the number of infertile couples seeking assisted
reproduction services for conceiving a child is increasing (Fideler& Bernstein, 1999).
The World Health Organization (WHO) estimates that in developing
countries there are 10 to 15% of couples of childbearing age, with an
increasing incidence in relation to age, that cannot bear a child by
natural methods, which means that 1 in every 7 couples is considered
infertile (Mascarenhas et al, 2012; Sembuya, 2010; Chachamovich, 2010).
Data from the Brazilian Institute of Geography and Statistics (IBGE)
shows that, in Brazil, there are approximately 4 million couples with
infertility (IBGE, 2010).
Infertility is
considered a disease of the reproductive system, defined by the absence
of clinical pregnancy after 12 months of regular sexual intercourse (US Department of Health and Human Services, 2014). The impossibility of conceiving a child has a significant impact on the health and well-being of the couple (Fideler& Bernstein, 1999), making it not only a problem of the private network, but a public healthcare issue now (Mascarenhas et al., 1990; Cui, 2010; Macaluso et al., 2010).
In many developed countries, the government finances human reproduction
treatments, especially in-vitro fertilization. Studies show that even
couples who have access to human reproduction services at the public
healthcare system face socioeconomic, racial, ethnic and financial
barriers to continue the treatment (Macaluso et al., 2010; Bitler & Schmidt, 2006; Chandra & Stephen, 2010).
In 2010, with the goal to facilitate access to human reproduction
treatment, Canada began to fund up to three cycles of in-vitro
fertilization per couple. Since then, there has been a change in the
socioeconomic profile of couples who started treatment at the public
healthcare system, increasing the number of unemployed, low income and
low educational level patients. The number of couples who sought
assisted reproductive treatment, through the public healthcare system,
because of secondary infertility, doubled after the deployment of this
healthcare policy (Togas et al., 2013).
Most infertility treatments performed in developing countries are
carried out at private clinics, and they are generally sought by older
patients, Caucasians, with low body mass index (BMI) and high
socioeconomic status, when compared to those seeking treatment at the
public healthcare system (Macaluso et al., 2010; Bitler& Schmidt, 2006; Chandra & Stephen, 2010).
There are about 106 fertility-treatment clinics registered by
Sisembrio/Anvisa of which only 8 are qualified to perform human
assisted reproduction procedures by the Public Healthcare System (SUS)
in Brazil. (Makuch et al., 2011; SisEmbrio2015).
Most of them are private, limiting access to treatment, and the cost is
still unmatched by the financial possibilities of most of the
population. In addition, public assistance programs do not always cover
all the costs of assisted reproduction care (Souza, 2014).
The public healthcare system should include human reproduction
treatment in their healthcare programs, ensuring the access for more
people.
The aim of the study was to evaluate the socioeconomic
profile and the main causes of infertility affecting couples seeking
assisted reproduction treatment through the public healthcare system in
the city of Campos dos Goytacazes. The assessment of this data should
contribute to the development of healthcare strategies and policies, in
order to facilitate access to high complexity infertility treatment at
the public healthcare system.
MATERIAL AND METHODS
We ran a
cross-sectional retrospective study, analyzing 600 medical records of
couples who sought the Infertility and Fetal Medicine Center at the
Alvaro Alvim Teaching Hospital in the city of Campos dos Goytacazes-RJ
from January 2008 to July 2014.
The records containing information on the variables were included in
this study. The records that did not have any information or had
incomplete data on the variables studied were excluded.
The patients were divided into three groups: GI, up to 35 years of age;
GII, 35 to 39 years; and GIII, aged greater than or equal to 40 years.
In each group we investigated the cause of infertility, the number of
children from spouses, women’s educational levels, family income and
the existence of previous unions.
The monthly income of the couple was based on the minimum wage value at
the time of the study, equivalent to U$ 253.40 and it was divided into
four groups: GI, couples with family income less than or equal to 1
minimum wage; GII, couples with family income between 2 and 3 wages;
GIII, couples with family income between 4 and 5 wages; GIV couples
with family income above six minimum wages. Any kind of prior marriage
or stable union was considered as previous marriage.
The causes of infertility were divided into groups: tubal factor 1,
patients with tubal ligation as a permanent method of contraception;
tubal factor 2, patients who had any obstructive pathology of the
tubes, except for tubal ligation; endometriosis, including any grade of
disease, all the way to superficial endometriosis in woman with absence
of clinical pregnancy after 12 months of regular sexual intercourse;
ovarian factor, patients with low ovarian reserve in woman with absence
of clinical pregnancy after 12 months of regular sexual intercourse,
premature ovarian failure, polycystic ovaries and anovulation; uterine
factor, patients with myometrium or endometrium pathologies such as
polyps and submucosal fibroids, intramural fibroids with an
intracavitary component or any size fibroids distorting the uterine
cavity, poor Müllerian formations and adhesions; male factor, made up
of patients with alterations in the semen analysis - according to World
Health Organization criteria of 2010. Among patients with male-related
factors, we evaluated the possible cause of infertility, such as the
presence of varicocele, vasectomy, testicular trauma, and other male
genitourinary tract diseases that contribute to changes in semen – such
as previous history of orchitis, testicular or epididymis tumors or
cryptorchidism.
There was a group of couples with unexplained infertility, established
when all other causes of infertility surveyed were excluded.
Any low complexity (timed intercourse, ovulation induction and
intrauterine insemination) or high complexity (in-vitro fertilization
and intracytoplasmic sperm injection - ICSI) treatment for infertility
held previously to the couple’s entry into the service was considered
as prior treatment.
To setup a database we used Microsoft Excel spreadsheet to plot the
data. Responses were numbered and participants were identified by means
of codes. The data was plotted and analyzed in the Minitab software,
version 15.1.1.0 (2007) and presented in graphs and tables plotted on
the Excel spreadsheet. Data was analyzed using descriptive statistics
and presented in the frequency of occurrence of each variable, to be
expressed in absolute numbers and percentage.
The study followed ethical procedures and was approved by the Ethics Committee of the School of Medicine of Campos.
RESULTS
From the 600 analyzed records, 37 were excluded because they did not
have any information or had incomplete data on the variables, and 563
were used in the study. From these, 2 patients chose to be a single
parent.
Eighty-five percent of the couples had not done been submitted to any
treatment for infertility, and 15% had had some kind of low or high
complexity treatment. Male factor was the cause of infertility in 34%
of the couples, and among the main causes for this male factor, 76% was
due to varicocele, 13% due to vasectomy, and other causes amounted to
13%. Tubal factor, due to tubal ligation was the cause of infertility
in 31,7% of the couples, and other tubal disorders corresponded to
16.3% of cases. Ovarian factor, endometriosis and uterine causes
accounted for 8.4%, 5.9% and 1.1%, respectively. Unexplained
infertility was the cause in 2.3% of these couples (Figure 1).
Regarding age, 56% of infertile women were under 35 years; 27% were
between 35 and 39 years of age, and 17% were 40 years old or more.
Regarding family income, 4.4% of the couples earned less than 1 minimum
wage, 58% had an income between 2 and 3 minimum wages, 25.8% between 4
and 5 minimum wages, and 11.7% of the couples had a monthly income
higher than or equal to 6 minimum wages (Figure 2).
Regarding the group of infertile women broken down by age, it was found
that those younger than 35 had the male factor as the main cause of
infertility, with 43,2% of cases, the majority (61.9%) earning between
2 and 3 minimum wages; they also had completed high school (45.5%) and
had no children (74%). We found that 23.4% had had previous marriage
and 57.5% had not been submitted to any previous treatment for
infertility. Among women 35 to 39 years old, the leading cause of
infertility was tubal factor - tubal ligation, corresponding to 38.8%
of cases in this age group; 52% earned between 2 and 3 minimum wages
monthly; 43.4% were high school graduates; 58.6% had no children and
22.4% had two children. Of them, 38.2% had had no prior relationship
and about 30% had previous treatment for infertility. Of patients over
39 years, the most common cause of infertility was tubal ligation
(42.9%); over half of them (55.1%) earned between 2 and 3 wages; 41.8%
had completed high school, 54.1% had no children, 22.4% had two
children and 13.3%, had one child only; 45.9% had no previous union and
17.1% had not been submitted to previous infertility treatment (Table 1).
Regarding the number of children among the patients receiving a minimum
wage or less, 76% had no children, 16% had two children and 8% three or
more. Of those who earned two to three minimum wages, 62.2% had no
children, 18.7% had two, 5.5% had three children and 1.2% had more than
three. Between 4 to 5 minimum wages, 66.3% had no children, 17.9% had
two, 9.7% and 2.1% had three and more than three children,
respectively. At the six or more wages range, 81.8% had no children,
9.1% had two and 7.6% had three or more children.
Upon associating education to infertility causes and number of
children, we found in patients with Junior High school degrees, the
main cause of infertility was tubal factor 1, with 49.7%, followed by
male factor with 23% of cases. Tubal factor 2, ovarian factor and
endometriosis were 18.6%, 5.0% and 2.5 %, respectively. 43.5% had no
children, 14.3% had one, 27.3% two, 11.2% three and 3.7 % more than
three children. Among patients who had completed High School, the main
infertility cause was the male factor (37.3%), followed by tubal factor
1 (30.9%) and tubal factor 2 (15.7%). 7.2% had an ovarian factor and
3.6% endometriosis. 7.5% had no children, 7.2 % had one, 18.5 % had
two, 6.4% and 0.7 % had three and more than three children,
respectively. Regarding Higher Education, the main cause of infertility
was the male factor (40.1%), followed by tubal factor 2 (14.4%).
Endometriosis and ovarian factor corresponded to 13.8 and 13.3%,
respectively; and tubal factor 1, 13.1% of cases. 88.8 % had no
children and nobody had more than three children in this group (Table 2).
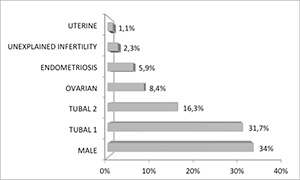
Figure 1. Main causes for the infertility treatment demand.

Figure 2. Profile of the average family income (%) of the surveyed couples.
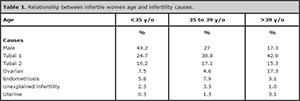
Table 1. Relationship between infertile women age and infertility causes.
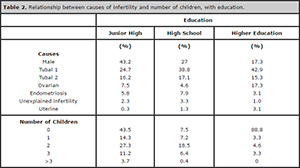
Table 2. Relationship between causes of infertility and number of children, with education.
DISCUSSION
Despite the spread of treatment methods, human reproduction is still
restricted to couples with better socioeconomic level, who can afford
the cost of treatment, since this remain the major impediment to
reproductive treatment access (Fideler& Bernstein, 1999; Macaluso et al., 2010).
A Canadian study evaluated the profile of patients who received human
assisted reproduction treatment before and after the country’s
government started to finance up to 3 cycles of in-vitro fertilization
for proven infertile couples (Macaluso et al., 2010).
Before the implementation of this healthcare policy in Canada, couples
seeking infertility clinics were mostly Caucasians, with high
socioeconomic level, higher educational level, higher family income,
low BMI and the women were older (Macaluso et al., 2010).
After the government policy, the profile of Canadian couples who were
seeking infertility treatment changed. The women were younger, with
lower family income and lower educational levels (Macaluso et al., 2010).
The changing profile reflects the large existing financial barrier
between couples and access to treatment, such observation corroborates
our data regarding the profile of couples who sought access to our
service.
The main infertility cause among American couples,
according to a study carried out in 2014 by the United States
Department of Health and Human Services, is the tubal factor followed
by the male factor (US Department of Health and Human Service, 2014).
The results obtained in our study reinforces the data found in the
American literature, as 47.7% of couples seeking this treatment had
tubal factor as a cause of infertility followed by the male factor,
with 34%.
In 2012, a study carried out to estimate the trend and
the prevalence of global and regional infertility since 1990, analyzed
household survey data obtained through the application of demographic
research and reproductive health questionnaires in several countries in
Europe, Asia and Africa (Mascarenhas et al., 2012). This study investigated both primary and secondary infertility.
There was little change in the prevalence of infertility between 1990
and 2010 in various regions of the world, except Africa and South Asia
where there was a marked decrease during such time period (Mascarenhas et al., 2012).
In areas where prevalence did not change much, there was an actual
decrease in fertility because fewer couples tried to have children.
The overall loss of fertility in women was mainly related to old age at
the time chosen to conceive a first child. They were usually women aged
over 35 years with higher socioeconomic level and higher education,
when compared to women with secondary infertility, who already had
children and had decreased fertility over the years.
In our study, we also found that the higher the monthly income of the
couple and the higher the educational level, the lower the number of
children. On the other hand, couples with more children were those with
lower socioeconomic status, lower family income and lower educational
level, as described on table 2.
Still, by sorting patients by family income, we found that the
difference in fertility rates was not significant among women under 35
years, 36-39 years and above 39 years of age in each group, showing
that in the same socioeconomic status, the infertility rate was similar
among younger and older women. Therefore, the factor that contributes
to the profile of patients seeking infertility treatment at the public
healthcare system is the socioeconomic status, especially the lower
status, nor the age factor as it happens in the private system (Figure 3). According to Mascarenhas et al,
this is so because the lower the socioeconomic status, the higher the
number of children, regardless of the woman’s age in these lower
socioeconomic tiers, secondary infertility being predominant, mainly by
tubal ligation (80%), which may reflect a policy of family planning
with conflicting concepts. While at higher socioeconomic levels, the
number of children is lower, and infertility occurs because of other
factors, such as planning children after professional success and
financial stabilization, with primary infertility as leading cause of
infertility in this group (Mascarenhas et al., 2012).
Still on the educational level, the presence of 43% of childless
couples in the group with junior high education may reflect the impact
of this change upon behavior in the planning of families. This is
supported by the observation that the number of children increases
parallel to family income. This observation of reproductive behavior
contrasts the outdated concept that infertility is a luxury of an elite
group and the least favored population need birth control due to the
number of children/family members. This data is consistent with the
observations of other studies and the Brazilian reality according to IBGE surveys (2010).
In 2009 the Department of Economic and Social Affairs of the United
Nations published fertility information from the world, age trends upon
first conception, number of children, contraception methods and family
planning (United Nations, 2011).
The results of this 2009 publication were similar to data released by
the WHO in 2011, linking the main cause of infertility in developing
countries, including Brazil, to tubal factor, and largely due to tubal
ligation, used as a contraceptive method (Mascarenhas et al., 2012; United Nations, 2011; OECD, 2015).
The explanation for these results is that in developing countries,
where most of the population is less socio-economically favored, women
have children at a younger age and the number of children is higher,
getting the final surgical sterility used as a contraceptive method in
wide scale and earlier (United Nations, 2011; OECD, 2015).
Over the years, most of these women engage in new relationships and
again have the desire of getting pregnant. On the other hand, in
developed countries, primary infertility plays an important role,
especially the older ones that plan their first pregnancy (Mascarenhas et al., 2012; United Nations, 2011; OECD, 2015).
This same study (United Nations, 2011)
showed that the highest percentage of tubal ligation is performed in
lower-income women with less education, being the leading cause of
demand for infertility treatment. In contrast, endometriosis and tubal
factor for other diseases of the tubes, except tubal ligation, are the
main causes of infertility in women with higher socioeconomic status (United Nations, 2011; OECD, 2015). These results were similar to those found in our study.
Our results also reflect this reality, although there is a behavioral
change in trend in the population, in terms of family planning these
concepts are active.
In Brazil there are 106 fertility clinics registered by
Sisembrio/Anvisa, of which only 8 are certified to perform human
assisted reproduction procedures by the Public Healthcare System (SUS) (Makuch et al., 2011; SisEmbrio 2015).
The waiting time for infertile couples to start treatment at the public
services is usually long, causing some services to often having to stop
servicing new couples in order to reduce the wait of those already
awaiting treatment (Souza, 2014).
Still, most
of these centers do not bear all expenses of infertility treatment
and/or do not offer the assisted reproduction techniques at all levels
of complexity. Even some couples starting treatment at the public
healthcare system (SUS) have to pay for essential laboratory tests,
afford the medication used, and they have restricted number of
induction cycles allowed (Souza, 2014).
Only in five human reproduction centers in Brazil patients do not need
to bear the cost of the stimulus protocol and they do not have limited
number of cycles to be performed (Makuch et al., 2011).
Our Infertility and Fetal Medicine Center at the Alvaro Alvim Teaching
Hospital, is one of those centers where treatment is fully paid by a
public program of municipal healthcare, although some supplemental
tests are not included.
Brazilian studies (Souza, 2014)
reported that another important factor of human reproduction in the
country is that not all couples have access to assisted reproductive
services by the public healthcare system, because the centers
themselves establish inclusion and exclusion criteria, or because most
of them are located in big cities, providing services only to couples
living in those regions, restricting access to many who live in remote
areas.
Data from the Demographic and Health Survey - 2006 (PNDS, 2009)
reported that in the last five years preceding the publication, 46% of
births derived from unplanned conceptions and other 18% from unwanted
conceptions. Although it corroborates events in countries where
assisted reproduction is part of a public assistance program, in
addition to the clear need for attention to these couples that have
their reproductive rights hampered, these data show a clear need for
implementation and intensification of public actions regarding
reproductive planning.
According to the Family Planning Act 1996
(Act 9263), Article 226, paragraph 2, one can understand that “family
planning is a set of fertility regulation actions that ensure equal
rights under the constitution, limiting or increasing the progeny of
women, men or the couple;” and among the specified actions listed on
paragraph 3, assistance in contraception and conception, making family
planning a set of global and comprehensive framework of actions. Thus,
according to the commitments established by the Constitution, based on
the principles of the SUS, it would be up to the State to provide the
treatment of both low and high complexity and bear the high cost of
assisted reproduction (Garcia et al., 2012).
The term reproductive planning seems to be more illuminating than the
usual “family planning” that can be confused with acts of “birth
control”. According to the National Demographic and Healthcare of
Children and Women17, an effective reproductive planning policy
offering clarification on contraceptive and conceptive methods, seems
to be the best way to improve reproductive assistance and change this
situation.
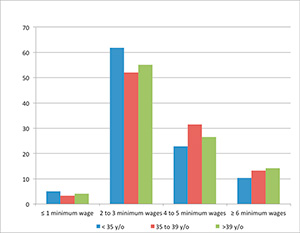
Figure 3. Relationship of couples seeking assisted reproduction
treatment through the public healthcare system in each group of women,
broken down by age (< 35; 35 to 39 years; and> 39 years)
according to family income.
CONCLUSION
The
profile of couples seeking the public healthcare system for infertility
treatment is: low-income, low education, having more children and the
tubal factor, due to tubal ligation, is the major cause of infertility.
The cost of treatment is still a limiting factor for most couples and
effective public healthcare policies could minimize the problem, since
it is still outdated and not comprehensive in this field.
The public healthcare system cannot meet all the demand, and
infertility treatment is restricted to a minority who can afford the
services on the private healthcare network. Reproductive rights and
their enforcement depend on access to reproductive planning services,
for both contraception and conception care. Public policy should be
adopted for the State to guarantee reproductive rights at all levels of
complexity.
REFERENCES
Bitler
M, Schmidt L. Health. Disparities and infertility: impacts of
state-level insurance mandates. Fertil Steril. 2006;85:858-65.
Medline Crossref
Chachamovich
JR, Chachamovich E, Ezer H, Flack MP, Knauth D, Passos, EP.
Investigating quality of life and health-related quality of life in
infertility: a systematic review. J Psychosom Obstet Gynaecol.
2010;31:101-10.
Medline Crossref
Chandra A, Stephen EH. Infertility service use among U.S. women: 1995 and 2002. Fertil Steril. 2010;93:725-36.
Medline Crossref
Cui W. Mother or nothing: the agony of infertility. Bull World Health Organ, 2010; 88:881–2.
Medline Crossref
Garcia
S, Bellamy M, de Russi K. Considerações sobre a reprodução assistida no
contexto brasileiro. In Anais do XVIII Encontro de Estudos
Populacionais. Águas de Lindóia, SP. 2012.
Link
Fideler AT, Bernstein J. Infertility: from a personal to a public health problem. Public Health Rep 1999; 114: 494–511.
Medline
IBGE – Instituto Brasileiro de geografia e Estatística - Brasil. Censo Demografico 2010. Available at: http://www.ibge.gov.br/home/estatistica/populacao/censo2010/default.shtm. Accessed: 27/08/2015.
Macaluso
M, Wright-Schnapp TJ, Chandra A, Johnson R, Satterwhite CL, Pulver A,
Berman SM, Wang RY, Farr SL, Pollack LA. A public health focus on
infertility prevention, detection, and management. Fertil Steril.
2010;93:16.e1-10.
Medline Crossref
Makuch
AY, Padua KS, Petta CA, Osis MJD, Bahamondes L. Inequitable access to
assisted reproductive technology for the low-income Brazilian
population: a qualitative study. Hum Reprod. 2011; 26:2054-60.
Medline Crossref
Mascarenhas
NM, Flaxman SR, Boerma T, Vanderpoel S, Stevens GA. National, Regional,
and Global Trends in Infertility Prevalence Since 1990: A Systematic
Analysis of 277 Health Surveys 2012; 9:e1001356.
Medline Crossref
OECD - Organisation for Economic Co-operation and Development (2011). OECD family database. Available at:http://www.oecd.org/els/family/database.html. Acessed 25 May 2015.
PNDS - Pesquisa Nacional de Demografia e Saúde da Criança e da Mulher – PNDS 2006 : dimensões do processo reprodutivo e da saúde da criança/ Ministério da Saúde, Centro Brasileiro de Análise e Planejamento. Brasília, Ministério da Saúde, 2009. Available at: http://bvsms.saude.gov.br/bvs/publicacoes/pnds_crianca_mulher.pdf Accessed 18/05/15.
Rutstein
SO, Shah IH. Infecundity, Infertility, and Childlessness in Developing
Countries. DHS Comparative Reports No. 9. Calverton, Maryland, USA: ORC
Macro and the World Health Organization; 2004.
Link
Souza
MCB. Latin America and access to Assisted Reproductive Techniques: A
Brazilian perspective. JBRA Assist Reprod. 2014; 18:47-51.
Crossref
SisEmbrio - 8º Relatório do Sistema Nacional de Produção de Embriões –. ANVISA. Available at: http://portal.anvisa.gov.br. Accessed 18/05/15
Togas T, King L, Zelkowitz P. Public Funding of and Access to In Vitro Fertilization. N Engl J Med. 2013; 368:1948-9.
Medline Crossref
United Nations, Department of Economic and Social Affairs, Population Division. World Fertility Report: 2009. United Nations Publication, 2011. Available at: http://www.un.org/esa/population/publications/WFR2009_Web/Data/WFR2009_Report.pdf.
US Department of Health and Human Service. National Public Health Action Plan for the Detection, Prevention, and Management of Infertility. Atlanta, Georgia: Centers for Disease Control and Prevention; June 2014. Available at: http://www.cdc.gov/reproductivehealth/infertility/pdf/drh_nap_final_508.pdf.