JBRA Assist. Reprod. 2017;21(3):222-229
ORIGINAL ARTICLE
doi: 10.5935/1518-0557.20170043
Blastocyst classification systems used in Latin America: is a consensus possible?
1Assisted Reproduction National Center INNAIFEST - Guayaquil - Ecuador
CONFLICT OF INTERESTS
The authors have no conflict of interests to report.
ABSTRACT
Objective: To identify different blastocyst classification systems used by embryologists in Latin American countries and evaluate the possibility of establishing a consensus among these countries.
Methods: An E-mail survey was carried out through the Latin American Network of Assisted Reproduction (REDLARA) aimed at embryologists from assisted reproduction centers in Latin countries.
Results: Sixty surveys were collected from 12 Latin American countries, of which 66.7% had >10years of professional practice as embryologists. Seven different blastocyst classification systems were reported, of which 5 have previously been described in the literature.
Conclusion: Although the group of embryologists surveyed use different blastocyst classification systems, most in this group consider that the embryo score system should be unified in their countries as well as in the region.
Keywords: blastocyst, consensus, Latin America
INTRODUCTION
The selection of the best embryo within a cohort of embryos is a crucial step for in vitro fertilization treatment (IVF) (Balaban et al., 2006; Santos Filho et al., 2012; Nasiri & Eftekhari-Yazdi, 2015). This has led to the development of different embryonic qualification systems, from morphological, biochemical and time-lapse systems (Richardson et al., 2015; Hossain et al., 2016); however, the system based on development rate and morphology assessment using light microscopy remains the embryo selection system mostly employed by IVF clinics worldwide (Alpha Scientists in Reproductive Medicine & ESHRE Special Interest Group of Embryology, 2011).
Several systems of morphological classification of embryos and blastocysts have been developed (Balaban et al., 2006; Mackenna et al., 2013; Hossain et al., 2016), from simple systems with one-degree assignment to complex systems using formulas to predict the likelihood of a pregnancy (Matsuura et al., 2010; Racowsky et al., 2010).
In the case of blastocysts, the evaluation and morphological classification usually considers the morphology of the inner cell mass (ICM), the morphology of the trophectoderm (TE) and cavity expansion (Balaban et al., 2006; Racowsky et al., 2010; Hill et al., 2013). Some of the systems published for classification of Blastocysts include Gardner (Gardner et al., 2000; 2004; Balaban et al., 2006), Veeck & Zaninovic (2003), Cecilia Sjoblom (Richardson et al., 2015).
Considering the variety of morphological systems for embryonic classification (Alpha Scientists in Reproductive Medicine & ESHRE Special Interest Group of Embryology, 2011), some countries and organizations have reached a consensus to standardize the morphological classification system of the embryos (Santos Filho et al., 2012).
Countries like the United Kingdom and Spain use a standardized national method of blastocyst classification (Hossain et al., 2016). In Spain, the Association for the Study of Biology of Reproduction - ASEBIR, published in 2015, the third edition of the ASEBIR Criteria for Morphological Assessment of Oocytes, Early Embryos and Human Blastocysts (ASEBIR, 2015). The Society for Assisted Reproductive Technology (SART) adhered to the embryo morphological evaluation system based on three categories: Good, Fair and Poor (Racowsky et al., 2010). The European Society of Human Reproduction and Embryology - ESHRE and the Alpha Scientist in Reproductive Medicine, reached a consensus to establish common criteria and terminologies for the classification of oocytes, embryos and blastocyst in Europe (Alpha Scientists in Reproductive Medicine & ESHRE Special Interest Group of Embryology, 2011).
No records were found regarding a consensus in terms of blastocyst classification systems in Latin America. Therefore, the present study aims to identify the different blastocyst classification systems that are used by embryologists in Latin American countries and evaluate the possibility of establishing a consensus among these countries.
MATERIALS AND METHODS
A survey was carried out via E-mail through the Latin American Network of Assisted Reproduction (REDLARA) aimed at embryologists from assisted reproduction centers in Latin America. This survey asked for information concerning the country where they practiced their profession, years of experience, the blastocyst classification system used and considerations regarding the unification of embryo score criteria.
RESULTS
Sixty surveys were collected from 12 Latin American specialists (Figure 1), of whom 66.7% had >10years of professional practice as embryologists, 21.7% from 5 to 10years and 11.7% <5years.
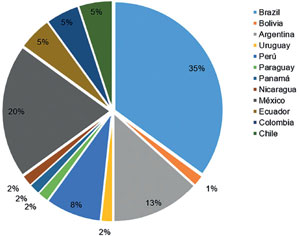
Figure 1. A: Countries where the embryologists surveyed work.
Seven different blastocyst classification systems (Figure 2) were reported among the embryologists surveyed. Five of these systems have been previously listed: Gardner and Schoolcraft (Table 1), Veeck (Table 2), ASEBIR (Table 3), Istanbul Consensus (Table 4) and Sjoblom (Table 5). In Brazil and Argentina, the Gardner system is the most used among the embryologists surveyed, while Mexican embryologists use the ASEBIR criteria (Figure 3).
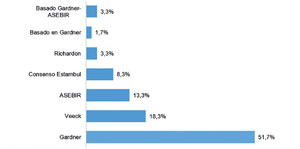
Figure 2. Blastocyst classification systems used among embryologists (Percentage).
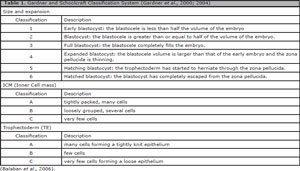
Table 1. Gardner and Schoolcraft Classification System (Gardner et al., 2000; 2004)
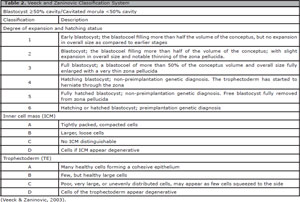
Table 2. Veeck and Zaninovic Classification System
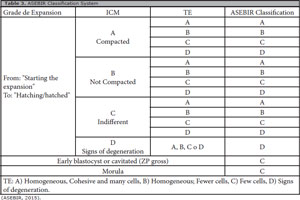
Table 3. ASEBIR Classification System
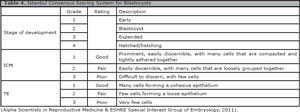
Table 4. Istanbul Consensus Scoring System for Blastocysts
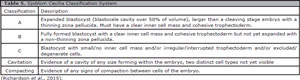
Table 5. Sjoblom Cecilia Classification System
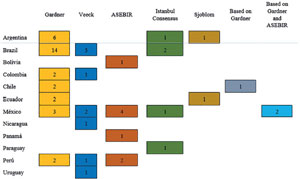
Figure 3. Number of Embryologists using the Classification systems reported.
Of the 5 previously published systems, the Istanbul consensus system has a numerical score, while the ASEBIR and Sjoblom systems are alphabetic. Gardner and Veeck systems are alphanumeric.
On a scale of 1 to 5 (1 easy and 5 difficult), 48.3% of the respondents considered that the blastocyst classification system used was easy, while 3.3% considered it difficult (Figure 4). In general, 48.3% of embryologists considered that the system they use to classify blastocysts could be simplified, while 51.7% believed that this was not possible.
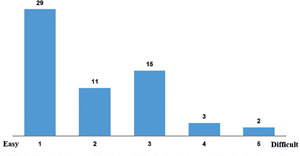
Figure 4. Difficulty Perceived Concerning the Blastocyst Classification System used: Number of embryologists.
88.1% of embryologists believe that the Blastocyst classification system should be unified in their countries and 88.3% think it should be for the entire region.
DISCUSSION
Since improvements in culture media gave the possibility of extending embryo culture until days 5 and 6 (Crosby & Mackenna, 2013; Richardson et al., 2015), the identification of the embryo that will become a viable blastocyst requires a robust scoring system (Gianaroli et al., 2012; Richardson et al., 2015). The classification system of embryos and blastocysts should be simple, composed of fields that are based on scientific research, with a predictive value tested and easily adaptable in laboratories (Racowsky et al., 2010).
Considering the variability of the embryo morphological classification systems published, several countries such as Spain as well as organizations such as SART in the United States and ESHRE in Europe have established consensus to standardize embryo qualification criteria for IVF treatments for assisted reproduction centers of those regions; however, no online published records about embryo consensus for assisted reproduction centers in Latin American countries were found.
From our survey, we collected 60 responses of embryologists from Assisted Reproduction Centers from 12 Latin American countries (Figure 1); However, we did not have responses from embryologists working in centers in Costa Rica, Guatemala, Dominican Republic and Venezuela, where there are also one or more centers accredited by REDLARA.
In the group of embryologists surveyed, seven different blastocyst classification systems were reported. The Gardner and Schoolcarft system is the most used among all embryologists surveyed (51.7%), being the main system used by embryologists from Argentina and Brazil. In Mexico and Peru there seems to be a greater variability in the use of blastocyst classification systems, with the ASEBIR score being the most used in Mexico (Figure 3). To assert this, it would be necessary to obtain information from a greater number of embryologists from the different countries of Latin America.
The survey also revealed the use of two unpublished blastocyst score systems. Two embryologists indicated the use of a standardized system based on the Gardner's and ASEBIR's criteria, while one embryologist reported the use of his own modified Gardner's system. Considering that the survey was anonymous, it was not possible to obtain information regarding the detailed criteria of these systems.
When comparing the five different criteria used by the surveyed embryologists, we can realize that there is variability in several points. The Istanbul consensus system is numerical, whereas ASEBIR and Sjoblom are alphabetic, and Gardner and Vecck are alphanumeric. Although the scoring criteria of the five systems already published include the expansion evaluation, the ICM and the TE of the blastocysts, the score for these characteristics has variations between the different systems (Table 6).
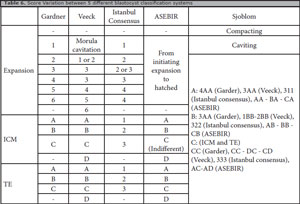
Table 6. Score Variation between 5 different blastocyst classification systems
In the case of expansion, the Gardner system includes a score of 1-6 evaluating the blastocyst from the start of the expansion (<50%, grade 1) to the hatched state (grade 6). The ASEBIR system also considers the expansion of the blastocyst from the beginning of the expansion; however, it does not give a score to this characteristic. In the Veeck's system, the score 1 would not correspond to Gardner's or Istanbul Consensus, because according to Veeck's characteristics, these embryos would be a cavitated morula. In addition, the Veeck system includes grade 6, given to hatching or hatched blastocysts, preimplantation genetic diagnosis.
Regarding the ICM and TE, ASEBIR and Veeck systems include the "D" score when they present degenerative cells. It should be noted that in the ASEBIR system, the "C" score of the ICM is indifferent in the final evaluation of the blastocyst and the TE has a greater importance.
Although the classification of blastocysts is based on the morphology of ICM, TE, as well as the expansion of the blastocyst cavity (Balaban et al., 2006; Racowsky et al., 2010; Hill et al., 2013), these classification systems may be difficult for patients to understand when discussing their embryonic quality prior to the transfer of an embryo (Heitmann et al., 2013). Therefore, other systems have been developed, such as the Sjoblom system, that considers the classification of the expansion, ICM and TE together, assigning A, B or C to the blastocyst score.
In general, 48.3% of the embryologists surveyed considered that the classification system used was easy (Figure 3), the rest considered that the difficulty of the systems was medium to high (Figure 5). It should be mentioned that the assessment of difficulty was not due to years of professional practice as an embryologist. Eighty-two percent of the embryologists who categorized their blastocyst qualification system with a difficulty of 3, 4 or 5, had over 10years of experience. Although potentially this could be irrelevant, because the survey assessed only the years in practice of an embryologist, not the time of experience in blastocyst classification.
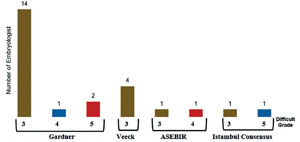
Figure 5. Qualification Systems with 3-4-5 level of perceived difficulty and number of embryologists.
Considering the variability of the score between the different blastocyst grading systems and possible inter-observer confusions that can present at the moment of blastocyst scoring with different systems, we asked about the possibility of unifying the embryo classification system in the region, in which 88.3% of the respondents agreed. However, it would be important to know who in this group of embryologists would be willing to modify their blastocyst classification system and adapt it to a common system for the region. This is a question that was not included in the survey.
Although this study includes only 60 embryologist responses, it gives precedence to investigate the probabilities of being able to establish a consensus regarding blastocyst score systems among Latin American countries, which should be based on the different classification systems used by assisted reproduction centers of our region. This consensus would provide the necessary recommendations for the centers and would be an important guide for assisted reproduction centers that have not yet established a fixed blastocyst qualification system. To achieve this, it would be convenient to collect more information on the different classification criteria of blastocysts used by our embryologists.
CONCLUSION
Seven different blastocyst classification systems were reported in 12 countries of Latin America. Although the group of embryologists surveyed use different blastocyst classification systems, most of them consider that the embryo score system should be unified in their countries as well as in the region.
REFERENCES
Alpha Scientists in Reproductive Medicine and ESHRE Special Interest Group of Embryology. The Istanbul consensus workshop on embryo assessment: proceedings of an expert meeting. Hum Reprod. 2011;26:1270-83.
Medline Crossref
Balaban B, Yakin K, Urman B. Randomized comparison of two different blastocyst grading systems. Fertil Steril. 2006;85:559-63.
Medline Crossref
Crosby J, Mackenna A. Blastocyst selection criteria: towards day five single embryo transfer. JBRA Assist Reprod. 2013;17:162-5.
Crossref
Gardner DK, Lane M, Stevens J, Schlenker T, Schoolcraft WB. Blastocyst score affects implantation and pregnancy outcome: towards a single blastocyst transfer. Fertil Steril. 2000;73:1155-8.
Medline Crossref
Gardner DK, Surrey E, Minjarez D, Leitz A, Stevens J, Schoolcraft WB. Single blastocyst transfer: a prospective randomized trial. Fertil Steril. 2004;81:551-5.
Medline Crossref
Gianaroli L, Racowsky C, Geraedts J, Cedars M, Makrigiannakis A, Lobo RA. Best practices of ASRM and ESHRE: a journey through reproductive medicine. Fertil Steril. 2012;98:1380-94.
Medline Crossref
Heitmann RJ, Hill MJ, Richter KS, DeCherney AH, Widra EA. The simplified SART embryo scoring system is highly correlated to implantation and live birth in single blastocyst transfers. J Assist Reprod Genet. 2013;30:563-7.
Medline Crossref
Hill MJ, Richter KS, Heitmann RJ, Graham JR, Tucker MJ, DeCherney AH, Browne PE, Levens ED. Trophectoderm grade predicts outcomes of single-blastocyst transfers. Fertil Steril. 2013;99:1283-9.e1.
Medline Crossref
Hossain A, Phelps J, Agarwal A, Sanz E, Mahadevan M. A Review of The Society for Assisted Reproductive Technology Embryo Grading System and Proposed Modification. Int J Fertil Steril. 2016;10:141-7.
Medline Crossref
Mackenna A, Crosby J, Zegers-Hochschild F. Sibling embryo blastocyst development as a prognostic factor for the outcome of day-3 embryo transfer. Reprod Biomed Online. 2013;26:486-90.
Medline Crossref
Matsuura K, Hayashi N, Takiue C, Hirata R, Habara T, Naruse K. Blastocyst quality scoring based on morphologic grading correlates with cell number. Fertil Steril. 2010;94:1135-7.
Medline Crossref
Nasiri N, Eftekhari-Yazdi P. An overview of the available methods for morphological scoring of pre-implantation embryos in in vitro fertilization. Cell J. 2015;16:392-405.
Medline Crossref
Racowsky C, Vernon M, Mayer J, Ball GD, Behr B, Pomeroy KO, Wininger D, Gibbons W, Conaghan J, Stern JE. Standardization of grading embryo morphology. Fertil Steril. 2010;94:1152-3.
Medline Crossref
Richardson A, Brearley S, Ahitan S, Chamberlain S, Davey T, Zujovic L, Hopkisson J, Campbell B, Raine-Fenning N. A clinically useful simplified blastocyst grading system. Reprod Biomed Online. 2015;31:523-30.
Medline Crossref
Santos Filho E, Noble JA, Poli M, Griffiths T, Emerson G, Wells D. A method for semi-automatic grading of human blastocyst microscope images. Hum Reprod. 2012;27:2641-8.
Medline Crossref
Veeck L, Zaninovic N. An Atlas of Human Blastocysts. New York, London: Informa Healthcare; 2003.