JBRA Assist. Reprod. 2015;19 (3):159-188
POSTER PRESENTATIONS
doi: 10.5935/1518-0557.20150036
Abstracts of the 19th Annual Congress of the SBRA, Búzios, RJ, 05-08 August 2015
P-01. Full Term Pregnancy in a Woman with Selective LH Deficiency
L. M. P. Sasaki1,2, B. R. de Carvalho1, H. M. Nagawa1, A. A. Silva1, L. A. Casulari3, A. Lofrano-Porto4,5
1GENESIS – Center for Assistance in Human Reproduction, Brasília, DF, Brazil
2Department of Obstetric and Gynecology, Faculty of Medicine, University Hospital of Brasília, University of Brasilia, DF, Brazil
3Neuroendocrinology Clinics, Endocrine Unit, University Hospital of Brasília, DF, Brazil
4Gonadal and Adrenal Diseases Clinics, Endocrine Unit, University Hospital of Brasília, DF, Brazil
5Molecular Pharmacology Laboratory, Faculty of Health Sciences, University of Brasília, DF, Brazil
INTRODUCTION: Selective luteinizing hormone (LH) deficiency has been described in only two women, who presented with normal pubertal development, but secondary amenorrhea and anovulation.
Both women harbored homozygous inactivating mutations in the LHB gene and their clinical presentation was predicted by the phenotype of lhb knock-out female mice.
In this animal model, exogenous human chorionic gonadotropin (hCG) administration rescued the ovarian expression of steroidogenic and ovulatory markers and provided normal response to exogenous gonadotropins induction, when compared to wild-type controls.
CASE REPORT: After informed consent, an individualized ovarian induction protocol with highly purified urinary hCG (hp-hCG) was performed in one of the previously described LH-deficient women, who harbored a homozygous IV2+1G>C mutation in the LHB gene.
She was 36 years old and had normal FSH levels and spontaneous development of small antral follicles, which exhibited growth arrest at the mid-follicular phase. In the first appointment, when a 14 mm follicle was identified by ultrasound, hp- hCG was started as 500 IU aliquots for daily subcutaneous administration.
Hormonal levels (FSH, estradiol, progesterone and beta-hCG), ovarian follicle growth and endometrial thickening were monitored during the following 9 days, after which, a 22 mm follicle was obtained.
Ovulation was, then, triggered by a single hp-hCG 5,000 IU dose, and patient was oriented to have intercourse every two days. Pregnancy was confirmed after 14 days.
Luteal phase support was provided from the second day after trigger until the end of the 12thweek with oral dydrogesterone, 30 mg/day, combined with subcutaneous hCG 500 IU dose every 3 days.
After an uneventful 40-weeks gestation, a healthy girl was born by cesarean section.
CoMMENTS: The reproductive outcome in this woman with selective LH deficiency phenocopied the findings in lhb knock-out female mice, in which impaired late follicular development was the most striking feature.
The treatment protocol we describe herein reinforces the efficacy of exogenous hCG on inducing late stages of follicular development, when FSH-dependent early follicular growth is assured. Moreover, it represents a valuable human model of assisted reproduction under controlled gonadotropin administration.
P-02. Embryo Transfer Medium Supplemented with 50% Serum Synthetic Substitute Improves Pregnancy Rates
C. O. Campos1, J. R. Campos2,3, N.C.S. Oliveira1, M. G. Cequinel1, C. A. Cornel1,4
1Embryo – Centro de Reprodução Humana, Curitiba, Brazil
2Clínica Genics Medicina Reprodutiva e Genomica, São Paulo, Brazil
3Rede Brasileira de Oncofertilidade
4Departamento de Tocoginecologia, Hospital das Clínicas - UFPR
OBJECTIVE: Evaluate the rates of biochemistry and clinical pregnancies after a period of embryos incubation in a transfer medium supplemented with 50% serum synthetic substitute (SSS) correlating the different times of exposure to the media and ages of the patients undergoing IVF-ICSI cycles.
MATERIALS AND METHODS: This study includes 367 patients, which 246 cases were from fresh embryo transfer cycles (ET) and 121 cases were from frozen-thawed embryo transfer cycles (FET).
The total sample was divided by age into three groups: up to 35 years, 36-38 years and equal to or greater than 39 years; and exposure time of embryos incubation in the transfer medium up to 5 minutes, from 6 to 10 minutes and over 10 minutes. The analysis of variables was performed using nonparametric Kruskal-Wallis test to calculate the differences between the groups (P <0.05 was considered statistically significant). It used the Sigma Plot software 11.2, Systat Software Inc.
RESULTS: We observed that embryonic exposure to transfer medium supplemented with 50% SSS up to 10 minutes improves the overall rates of biochemical pregnancy (FET: 46%) and clinical pregnancy (ET: 39%, FET 36%) p <0.05.
The group of patients up to 35 years also showed improvement in biochemical pregnancy rates (FET: 54%) and clinical pregnancy rates (ET: 38%, FET: 42%) p <0.05, after embryonic exposure up to 10 minutes.
Patients aged 36 to 38 showed improvement in the biochemical pregnancy rates (ET: 64%, FET: 50%) and clinical pregnancy rates (ET: 59%, FET: 25%) p <0.05, when the embryos were exposed during a period of 6 10 minutes, compared to other exposure times. The group of patients 39 years or older showed improvement in overall clinical pregnancy rate (29%) when the embryos were exposed during a period of 6 to 10 minutes, P <0.05.
CONCLUSIONS: Increasing the protein supplementation on embryo transfer medium, which is commonly supplemented with 10% or 20% SSS, for a concentration of 50% is beneficial and significantly improves pregnancy rates and it can be implemented safely in laboratorial routine.
P-03. Assessment of the Potential of Different Culture Media to induce Oocyte Maturation in vitro
E. S. de Araújo1, R. A. Salvador1, D. Til1, T. M. Pereira1, M. D. Da Silva1, V. L. L. Amaral1
1Universidade do Vale do Itajaí –SC (UNIVALI)
OBJECTIVE: The present study tested different commercial media with the objective to evaluate the in vitro oocyte maturation.
MATERIALS AND METHODS: Ovaries were collected from F1 female mice (Balb/C x C57Bl/6) at two months of age, and dissected in Human Tubal Fluid (HTF-Modified - Irvine®) supplemented with 10% Serum Substitute Supplement (SSS-Irvine®), to obtain the oocytes. These were denuded, and those with a germinal vesicle (GV) were selected, distributed and incubated at 37°C under 5% CO2 for 24 hours in the following media: Single Step Medium (SSM-Irvine®) + 10% of SSS; Global (Lifeglobal®) + 10% SSS; G1 Plus (Vitrolife®); G2 Plus (Vitrolife®); G1 (Vitrolife®) + 10% SSS; G2 (Vitrolife®) + 10% SSS; Blast RBC (Ingamed®) + 10% SSS; GV Fert (Ingamed®); IVF (Vitrolife®) + 10% SSS and IVF Plus (Vitrolife®).
RESULTS: After 24 hours, the oocytes that reached the metaphase II stage were counted in the various culture media, as a measure of the maturation potential of the medium. Maturation rates of each medium and combinations, were in descending order 62.96% for G1 + SSS (17/27); 52% (13/25) to SSM + SSS; 48.15% (13/27) for GV Blast + SSS; 45.16% (14/31) for00Fert + SSS.
CONCLUSIONS: The results show that the G1 + SSS medium has the greatest potential to promote oocyte maturation, followed by SSM and SSS + GV Blast + SSS means. This study demonstrated that the culture medium can be a limiting factor for maturation in vitro, even without hormone supplementation or other components.
P-04. Analysis of Roc Curve to Define the Best Clinical Parameters to Correlate with Pregnancy in In Vitro Fertilization Cycles
A. K. Bartmann1, V. C. P. S. Nascimento1, M. Faria Junior2, L. L. M. da Silva1, G. P. de Barros1, L. S. de Paula1
1Clinica Ana Bartmann - Centro de Reprodução Humana/ UNAERP
2Universidade de Ribeirão Preto – UNAERP
OBJECTIVE: To define the best clinical parameters related to attaining pregnancy in in vitro fertilization cycles.
MATERIAL AND METHODS: One hundred twenty-one cases of in vitro fertilization were assessed according to: patient age, Antral Follicle Count (AFC), Mature Follicle Count (MFC), Follicular output rate (FORT), number of oocytes collected and embryos obtained according to the positive (pregnancy) or negative (non-pregnancy) outcome. All patients underwent the same ovarian stimulation protocol and received daily doses of gonadotropins between 225 and 300 IU/day. The existing relationship between each parameter and pregnancy/non-pregnancy was analyzed by plotting an ROC curve, with the Youden index (J) being used to determine sensitivity and specificity values. The Medcalc V.15.2.2 software was utilized for that purpose.
RESULTS: Through the analysis of the ROC curve, we were able to observe that the best parameter to differentiate the binomial states of pregnancy and non-pregnancy was the number of embryos obtained, with an ROC curve area of 91.7, p<0.0001, sensitivity of 72.73% and specificity of 95.45%. The second-best parameter was the Mature Follicle Count, with an ROC curve area of 88.8, p<0.0001, sensitivity of 72.73% and specificity of 90.91%.
The third-best parameter was the number of oocytes captured, with an ROC curve area of 88.1, p<0.0001, sensitivity of 72.73% and specificity of 90.91%. The fourth-best parameter was the FORT with an ROC curve of 82.2, p<0.0001, sensitivity of 81.82% and specificity of 69.32%. Later we carried out the Antral Follicle Count, with an ROC curve area of 77.3, p<0.0001, sensitivity of 81.82% and specificity of 60.23%.
Surprisingly, age was shown to be the worst pregnancy indicator, with an ROC curve area of 70.1, p=0.0001, sensitivity of 69.7%, and specificity of 62.50%.
CONCLUSIONS: According to the areas under the ROC curve, one can conclude that the number of embryos obtained in a fertilization cycle, if taken isolatedly, is the best factor related to attaining pregnancy.
P-05. Euploidia Rate in Embryos Undergo Genetic Screening Pre Implantation on Different Days of Development and its Correlation with Maternal Age
V. Rosa1, J. A. Lucca Neto1, A. Schuffner1
1Clínica Conceber – Centro de Medicina Reprodutiva – Curitiba - PR
OBJECTIVE: To evaluate the rate of euploid embryos identified by pre implantation genetic screening and its relationship with maternal age; and pregnancy rate of euploidy embryos in our facility.
MATERIAL AND METHODS: In this study, we used 188 embryos from 60 controled stimulated cycles, carried out between 2011 and 2015. Were used embryos in cleavage stage (D3) and blastocysts (D5, D6, D7) biopsied and analyzed for 24 chromosomes (CGH-array and NGS). Moreover, the pregnancy rate of euploid embryos was evaluated. Statistical analysis was performed by chi-square test.
RESULTS: The average rate of euploid embryos was 23.4%. There was no significant difference in euploidy rate combining age groups, it was respectively 27.3%, 23.4% and 20.9% for patients younger than 30 years; 35-39 years; and 40 years or older (p = 0.78). We did not observe significant differences in euploidy rate when compared biopsied embryos on different days of development (p = 0.31), it was respectively 16.7%; 27.9% 22.2% and 0% for biopsies in D3; D5; D6 and D7. The clinical pregnancy rate in our service withr euploid embryos transferred was 42.9%.
CONCLUSIONS: Although there was no significant difference when comparing different age groups, the data suggest that younger patients seems to produce more euploid embryos. Ideally, blastocysts able to be biopsied must have critical morphological characteristics such as high degree of expansion, presence of hernia and high number of trophoectoderm cells; When these characteristics are present on the fifth day of development, there is a greater chance that these embryos are euploid.
P-06. Assessment of Oocyte and Embryo Quality of Poor Responders After the Administration of Growth Hormone (GH) as a Co-Adjuvant for Ovarian Stimulation in IVF-ICSI Cycles
C. O. Campos1, C. A. Cornel1,2, M. G. Cequinel1, N. C.S. Oliveira1, W. P. Martins3, A. C. J. S. Rosa e Silva3
1Embryo – Centro de Reprodução Humana, Curitiba, Brazil
2Departament of Tocoginecology, Federal University of Paraná, Brazil
3Department of Ginecology and Obstetrics, School of Medicine of Ribeirão Preto, Brazil
OBJECTIVE: Evaluate oocyte and embryo quality from poor responders patients undergoing ovarian stimulation for IVF-ICSI cycles after the use of growth hormone (GH).
MATERIALS AND METHODS: This pilot study included 26 patients, which 19 patients were the control group: aged ≥ 40 years, three or fewer follicles in the first cycle of IVF-ICSI and impaired ovarian reserve, and 7 patients were the group under use of GH: aged ≥ 40 years, prior cycle with three or fewer follicles recovered, low fertilization rate, poor oocyte and embryo quality and impaired ovarian reserve. The parameters used to evaluate oocyte quality were: the average of cumulus oophurus diameter, morphological characteristics of polar body (PB), cytoplasm, perivitelline space (PS), zona pellucida (ZP), general morphology and fertilization rate; and to evaluate embryo quality were: cleavage rate, number and regularity of blastomeres and anuclear fragmentation rate. The age and cumulus diameter were analyzed using the Mann-Whitney test and the other variables by χ2 test (P <0.05 considered statistically significant).
RESULTS: Regarding median of patients ages was 36 years (DIQ 34-39) on control group and 38 years (DIQ 35-39) on GH group (P=0.27). The analysis of mean cumulus diameters resulted in median of 887μm (DIQ 738-1205) and 810μm (DIQ 641-946) for control and GH groups, respectively (P=0.49).
Parameters of oocyte morphology were classified as normal, altered or completly altered and the results found were not significant when compared between groups (PB: p=0.53; Cytoplasm: p=0.70; PS: p=0.63; ZP: p=0.24; general morphology: p=0.54). Fertilization and cleavage rates and development of good quality embryos on day 2 did not show significant differences between groups (p=0.92; p=0.65 and p=0.91 respectively).
CONCLUSIONS: We observed in these preliminary findings that there was no significant difference in oocyte and embryo quality among patients using or not GH. We consider the fact that the results were no significant due to the small sample, because it is a pilot study, since in our laboratory routine and the world literature found clinically favorable results in patients who used GH as co-adjuvant for ovarian stimulation in IVF-ICSI cycles.
P-07. NAS: Difficulties and challenges experienced in its applicability in an Assisted Human Reproduction Center of the city of São Paulo: Experi-ence Report
S. P. C. Roque1, H. Storti1, M. Ferrari1, J. Assi1, C. T. Kimati1
1Huntington Centro de Medicina Reprodutiva – São Paulo – Brasil
INTRODUCTION: The Nursing Assistance Systematization (NAS) is one way that nurses use to apply their scientific and human knowledge in healthcare practice, prioritizing patient care. The Assisted Human Reproduction is a very specific area of expertise, with a view to improvements in nursing process, we seek to identify the difficulties and challenges experienced in implementing the NAS in a center for assisted human reproduction.
CASE REPORT: To assist in the gathering of information, a questionnaire with open and closed questions was prepared, and applied to nurses who participated in the NAS implementation process in a center of human reproduction. The questions addressed the relevance, degree of difficulty in the implementation of the nursing staff membership, major challenges encountered and suggestions for improvements.
COMMENTS: All the nurses considered relevant the application of NAS; 57.13% considered medium degree of difficulty in the implementation; and 57.14% considered satisfactory the accession of the team. The lack of physical space and the consequent impossibility of closer contact with the patient was the most cited factor as difficulty in the implementation of NAS, but not characterized impediment in implementation. Although there is a prevailing tendency to implement the NAS in specific areas of expertise, it is expected to approach the subject in this study encourage nurses to initiate this process.
P-08. Evaluation of the Follicular Concentration of Vitamin D on the day of Oocyte Retrieval in a Brazilian population of Women undergoing ICSI
V. D. A. Silva1, R. A. Antunes1,2,3, P. Areas3, E. Bloise1, M. C. Borges de Souza3, T. M. Ortiga-Carvalho1
1Laboratório de Endocrinologia Translacional, Instituto de Biofísica Carlos Chagas Filho, Universidade Federal do Rio de Janeiro
2Maternidade Escola, Universidade Federal do Rio de Janeiro. Rio de Janeiro, Brasil
3Clinica Fertipraxis Rio de Janeiro, RJ, Brasil
OBJECTIVE: Vitamin D deficiency has been largely related to infertility in animal models. However, data demonstrating a direct association between hypovitaminosis D and human infertility are still conflicting. Increased body weight and body mass index (BMI) are known factors associated with infertility. In this context, incidence of hypovitaminosis D rises as body weight increases. Therefore, we hypothesized that increase in body weight and BMI would be associated with lower 25-hidroxyvitamin D (25[OH]D) levels in the follicular fluid (FF) of patients undergoing infertility treatments, more specifically, in patients enrolled in intracytoplasmic sperm injection (ICSI) protocols. Thus, our objective herein was to assess FF levels of 25(OH)D from women undergoing ICSI and compare FF (25[OH]D) levels with different causes of infertility, body weight and BMI.
MATERIAL AND METHODS: In order to investigate if FF (25[OH]D) levels are associated with female weight and different causes of infertility, FF aspirates were collected after oocyte aspiration procedures, from 199 patients undergoing ICSI. 25(OH)D levels were assessed by chemiluminescence. Etiology of infertility was defined with clinical history and follow up. Data were analyzed by Student-t-test, differences were considered to be significant at a P≤0.05.
RESULTS: Since 25[OH]D deficiency is defined as serum concentrations below 20ng/ml, we investigated in our cohort, the number of women with lower FF levels of 25[OH]D. 71 women had FF levels of 25(OH)D lower than 20ng/ml (35,7%), whereas 128 women had FF levels of 25(OH)D higher than 20ng/ml (60,8%). Patients with lower FF 25(OH)D levels had increased weight (64,1kg) compared to patients with higher 25(OH)D levels (60,7kg, p<0.05). No differences in FF 25(OH)D levels were observed when comparing etiology of infertility or BMI in both
subject groups.
CONCLUSIONS: FF levels of 25(OH)D were decreased in patients with higher weight, confirming our hypothesis. Future studies should investigate the specific role of vitamin D and assess whether Vitamin D replacement would have positive effects circumventing infertility.
P-09. Results obtained with embryos transferred two days after thawing
G. G. de Oliveira1, L. P. de Aguiar1, A. S. Rodrigues1, E. M. Brescia1, C. O. S. C. Lopes1, L. A. M. de Moraes1
1Clínica Fertibaby –Belo Horizonte –MG - Brasil
OBJECTIVE: To compare rates of pregnancy and implantation of patients whose embryos were vitrified and transferred on the third day of cultive and patients whose embryos were vitrified on the third day of cultive and transferred two days after thawing (fifth day of embryonic development).
MATERIAL AND METHODS: A total of 110 patients were selected with age ≤ 35 years, from January 2014 to December 2014 that received vitrified embryos on the third day.
Patients from Group A received embryos thawed and transferred on the same day (third day of cultivation); while patients of Group B have thawed embryos on the third day and cultivated for two more days (on the fifth day of development). The freezing method was vitrification (Ingámed®). Test T Student was used for comparison between ages of groups and X2 test for comparison between pregnancy and implantation rates.
RESULTS: The average age of patients in Group A was 31,58 ± 2,95 and Group B was 29,43 ± 4,33; P=0,07. The pregnancy rate of Group A was 37,67% and Group B was 47,05%; P=0,46. The implantation rate in Goup A was 21,19% and in Group B was 25,92%; P=0,54.
CONCLUSIONS: Despite the fact that there was no estatistical significance, to postpone embryo culture for two more days, before the embryo transfer, could be an alternative for patients whose embryos were vitrified on the third day of cultivation.
P-10. Is Response to Controlled Ovarian Stimulation for IVF Associated with ABO Blood Type?
T. Rassi1, P. Galvão1, H. M. Nakagawa1, A. A. Silva1, A. C. P. Barbosa1, B. R. de Carvalho1
1GENESIS – Center for Assistance in Human Reproduction, Brasília, DF, Brazil
OBJECTIVE: To investigate whether there is any association between ABO blood type and ovarian response to controlled stimulation for in vitro fertilization (IVF).
MATERIAL AND METHODS: This retrospective analysis included 197 patients undergoing controlled ovarian stimulation for IVF cycles, in a Brazilian private center for assistance in human reproduction, between January and December 2014. Firstly, patients were allocated in age groups: (I) ≤ 35 years, n = 88; (II) 36-40 years, n = 82; and (III) > 40 years, n = 27. Patients were, then, sub-grouped, based on blood type: A, B or AB, and O. The total number of oocytes and the number of mature oocytes retrieved were considered as primary outcomes. Analysis of variance (ANOVA) was used to compare means, and Chi-square tests to compare percentages between ABO blood types within groups.
RESULTS: Distributions of blood types by age group were as follows: (I) A, 45.4 %; B or AB, 14.8%; O, 39.8%; (II) A, 40.3 %; B or AB, 13.4%; O, 46.3%; and (III) A, 29.7 %; B or AB, 14.8%; O, 55.5%. Within each age group and based on ABO blood type, no significant differences were found in the total number of oocytes [(I) A, 12.2 ± 8.2; B or AB, 13.9 ± 11.4; O, 13 ± 8.3; (II) A, 8 ± 5.2; B or AB, 8 ± 4.2; O, 8.2 ± 5.2; and (III) A, 6.4 ± 3.4; B or AB, 4.7 ± 3.9; O, 7.4 ± 5.5; p > 0.05 for all analyses] or mature oocytes retrieved [(I) A, 9.6 ± 6.9; B or AB, 12 ± 9.9; O, 10.2 ± 6; (II) A, 6.5 ± 4.2; B or AB, 7 ± 3.3; O, 6.5 ± 4.1; and (III) A, 5 ± 2.7; B or AB, 2.5 ± 2.5; O, 5.5 ± 4.3; p > 0.05 for all analyses].
CONCLUSIONS: Our study suggests no association between ABO blood type and ovarian response in patients undergoing stimulation for IVF. Controversies on the predictive value of ABO blood type in determining ovarian stimulation response still remain.
P-11. Preservation of Fertility in Cancer Patients: A Reality?
J. F. Dos Santos1, M. S. Borges1, G. M. Coelho1
1Instituto Valenciano de Infertilidade (IVI - Salvador) -Brasil
OBJECTIVE: To evaluate the rate of patients who have resorted to fertility preservation before starting treatment against cancer in a reference clinic in Salvador.
MATERIAL AND METHODS: We studied retrospectively all cases of cryopreservation of cancer patients 2010 to May 2015, evaluating the frequency of cryopreservation procedures during the stipulated period and in relation to the success or failure of pregnancy.
RESULTS: It was observed that the preservation of fertility in patients, either through cryopreservation of oocytes and embryos and sperm increased significantly over the years. The preservation of male fertility was most frequent in relation to women in cases of cancer patients.
CONCLUSIONS: The preservation of male and female fertility is an increasingly growing strategy in oncology setting prior to treatment with chemotherapy or radiation. Practice has given fertility hope for many young men and women, cancer survivors with desire to have their own biological children.
P-12. Pregnancy Rate after Embryo Transfer According to Number and Morphology of Available Embryos
C. M. da Luz1, M. A. Coelho Neto1, V. S. I. Giorgi1, W. P. Martins1, R. A. Ferriani1, P. A. A. S. Navarro1
1Setor de Reprodução Humana, Departamento de Ginecologia e Obstetricia, Faculdade de Medicina de Ribeirão Preto - USP
OBJECTIVE: Evaluate the clinical pregnancy rate in fresh transfer of cleavage stage embryo according to the number of embryos formed and the presence or absence of transference of top quality embryo (TQE).
MATERIAL AND METHODS: We conducted a retrospective cohort study. Between January 2011 and December 2012, the records of all women undergoing controlled ovarian stimulation (COS) for ICSI, aged ≤40 years and with at least one formed embryo were evaluated. The women were stratified into 3 groups according to the number of embryos formed in cleavage stage (1 embryo; 2-3 embryos and ≥ 4 embryos). In each stratum, we compared the age, body mass index (BMI) and clinical pregnancy rate among those who have or have not formed at least one TQE to be transferred in the fresh cycle: 4 cells Grade 1 (symmetric blastomeres with less than 10% fragmentation and without multinucleation) to transfer on D2 or 8 cells Grade 1 to transferred D3. Comparisons were made by the relative risk or mean difference with their 95% confidence intervals.
RESULTS: During the study period, 787 women were subjected to COS for ICSI and 633 had at least one embryo to be transferred in the same cycle. Within each stratum, we did not observed significant difference in age and BMI among women with and without TQE. However, the clinical pregnancy rates per transfer were higher in the group with TQE, being statistically significant in the group with ≥4 embryos formed (Table 1).
CONCLUSIONS: Considering the women that form a similar number of embryos, particularly those that develop four or more embryos, those which form and transfer embryos of excellent morphology has more chance to reach a clinical pregnancy.
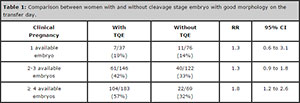
Table 1: Comparison between women with and without cleavage stage embryo with good morphology on the transfer day.
P-13. Influence of Oocyte Vitrification Technique in Levels of Expression of BAX, BCL2, IDH2 and ZP3 Genes
C. P. P. Molina1, L. C. C. da Silva1, L. A. Batista1, Thaís T. Higa1, A. C. J. Sá Rosa e Silva1
1Department of Obstetrics and Gynecology - School of Medicine of Ribeirão Preto, University of São Paulo, Ribeirão Preto, SP, Brazil
OBJECTIVES: Considering the importance of vitrification techniques in the clinical practice, the aim of this study was to evaluate the effects of vitrification in the expression of some oocyte quality markers genes. The factors related to the regulation of apoptosis, BCL2 (B-cell lymphoma 2) and BAX (BCL2-associated X protein), to maturation and oocyte protection IDH2 (NAPH+ dependent isocytrate desidrogenase) and the primary receiving the sperm (Zone pellucida sperm-binding protein 3 (ZP3) were evaluated for the mRNA levels in bovine oocytes matured in vitro and/or cryopreserved.
MATERIAL AND METHODS: Complex cumulus-oophurus (COCs) were matured in medium TCM 199 containing fetal bovine serum, hormones (FSH and LH) in an 5% CO2 atmosphere, at 38,5ºC during 24 h. Oocytes were denuded and stored in RNA protective solution (RNA later), or vitrified in stepwise vitrification procedure using Glycerol and Ethylene Glycol solutions (10, 30 and 50%), thawing and stored. Subsequently, the oocytes were subjected to RNA extraction, cDNA was synthesized, preamplified, and the level of expression of the BAX, BCL2, IDH2 and ZP3 genes was evaluated by real time PCR. The statistical analysis was performed using SAS® 9.2 software and the Mann-Whitney test was applied.
RESULTS: No statistically significant difference of IDH2 and ZP3 mRNAs levels were observed in oocytes non-vitrified and vitrified. However, BAX and BCL2 mRNA levels were greater in oocytes non-vitrified compared to vitrified group.
CONCLUSIONS: During vitrificatioon, oocytes are subjected to different conditions that can cause oxidative stress and/or thermic, changing the levels of mRNA and, consequently protein function. The BCL2 and BAX genes are important regulators of apoptosis, of great importance in elucidating the mechanisms of cellular damage secondary to cryopreservation processes. This study demonstrated that vitrification technique used altered mRNA levels of BCL2 and BAX genes. Once other studies have demonstrated that the reason BAX / BCL2 defines the future development of the oocyte, FIV studies vitrified oocytes may inform the altered expression of BCL2 and BAX interferes with fertilization thereof.
P-14. Reduction of Fetal Bovine Serum Concentration in the Medium of In Vitro Maturation of Oocyte and their Influence on Embryonic Production
C. P. P. Molina1, L. A. Batista1, C. G. Verruma2, R. A. Vila2, R. B. Lôbo2, A. C. J. de Sá Rosa e Silva1
1Department of Obstetrics and Gynecology - School of Medicine of Ribeirão Preto, University of São Paulo, Ribeirão Preto, SP, Brazil
2Departamento of Genetics - School of Medicine of Ribeirão Preto, University of São Paulo, Ribeirão Preto, SP, Brazil
OBJECTIVES: Largest oocyte maturation rates are obtained with the addition of protein sources in the maturation medium, one of the fetal bovine serum (FBS). Already for the developing embryo, these beneficial effects are seen with growth factors, chelating of heavy metals and components that assist in expanding cumulus cells. However, the use of FBS may cause changes in ultra structure and mRNA expression, compaction and embryonic blastulation, while increasing the concentration of fatty acids and cytoplasmic lipid droplets, lower the cryotolerance and contaminate the medium. Therefore, the objective was to reduce the amount of serum in vitro maturation medium (IVM), without interference in embryonic production in order to reduce possible damage caused by the serum, which can generate impact in the oocyte cryotolerance.
MATERIAL AND METHODS: Complex cumulus-oocyte were matured in TCM 199 containing 10% (G10; N=364) or 5% (G5; N=366) fetal bovine serum, 0,5μg/ml FSH, 5 μg/mL LH, and 1 μg/mL 17β-estradiol, with 5% CO2, 38,5ºC for 24 h. After IVM, oocytes were submitted to the in vitro fertilization (IVF) in medium supplemented with 20 μg/mL heparin and 6 mg/mL fatty acid-free albumin from bovine serum (BSA). After fertilization, the presumptive zygotes were cultured with cumulus cells in CR2 medium containing 10% fetal bovine serum and 3 mg/mL BSA until 224 h post-insemination. Data analysis was done by Qui-Quadrado.
RESULTS: The reduction of fetal bovine serum in the in vitro maturation did not interfere in cleavage rates and in vitro embryos when compared to the control group, and the 71.86% of cleavage (G10) and 73.35% G5) (p>0,05) and blastocyst formation rates of 42.03% (G10) and 45,90% (G5) (p>0,05), respectively.
CONCLUSIONS: Despite the serum be in the essential component in vitro maturation medium, its reduction did not interfere in the oocytes ability to produce embryo.
P-15. Case Report: Correlation Between Body Fat Composition, Body Mass Index and Seminal Oxygen Reactive Species in Infertile Men
C. Ranéa1, J. R. Pariz1,2,3, R. A. C. Monteiro1, I. Ciccone4, J. Hallak1,2,3
1Laboratory Androscience, SP-SP
2Sector of Andrology, Department of Urology FMUSP, SP-SP
3Unit of Reproductive Toxicology, Department of Pathology, FMUSP, SP-SP
4Nutrition Sector JH Clinic, SP-SP
INTRODUCTION: Male infertility is multifactorial by environmental factors, habits and lifestyle (calorie intake and low nutritional value) and genetic factors. This case study illustrate the need for a multidisciplinary, more specific and comprehensive approach in the health of the patient seeking more than the recovery of fertility, global human health.
CASE REPORT: Patient 38 years, married for two years, planning pregnancy for 18 months, sent the clinic for presenting primary infertility. Research fertility began with semen analysis and sperm function tests, which were measured reactive oxygen species (ROS) seminal (1.32x10⁴ cpm / 20x106 sperm), body mass index (BMI = 28.70kg / m•), body fat (26.80 kg), total progressive motility (0%) and total motility (30%). As for genetic analysis, no Y chromosome microdeletions was observed. The patient was diagnosed with bilateral varicocele and forwarded to varicocelectomy. After microsurgery, the patient has worsening of semen. The specific metabolic examination diagnosed nutritional deficiency Hypovitaminosis “D’’ or recurrent metabolic dysfunction of the adrenal stress. Patient returns to the lab again with decrease in semen quality, very high cortisol and symptoms of fatigue.
The approach adopted was diet, medical treatment and cryopreservation.
After the treatment period established by the physician, the patient returns with 10kg less (BMI=28.80, unchanged; body fat=19.40kg, reduction of 7.4kg) and reports to be without fatigue and stress.
In the seminal analysis showed an increase of progressive motility (20%) and total motility (35%), with levels of ROS unchanged (1.32x10⁴ cpm/20x106 sperm).
COMMENTS: In the present study, we exposed a case to demonstrate the multifactorial assessment of the man. The conduct adopted with varicocelectomy and nutritional intervention had success as an improvement of sperm motility. The patient presented significant reduction of body fat mass, with no change in BMI after nutritional education.
These data also suggest that BMI, although widely used, is a poor indicator to measure obesity and that there is a strong correlation between fat accumulation and sperm motility.
P-16. The Role of the Nurse Educator in a Reproductive Medicine Center of São Paulo: Experience Report
J. Assi1, M. Ferrari1, C. Kimati1
1Grupo Huntington Centro de Medicina Reprodutiva
INTRODUCTION: According to the World Health Organization, 8-10% of couples will experience the experience of infertility. The care infertile couple in Human Reproduction centers (HR) is developed by a multidisciplinary team, involving doctors, biologists, biomedical, psychologists, nutritionists, pharmacists and nursing staff. The role of the nurse educator is indispensable, since this area is, in general, little known by the nursing staff.
CASE REPORT: The purpose of conducting a study on continuing education, with the nursing team in a HR specialist private institution appeared before the practice teaching experience. This specialty is little or not addressed during the technical level courses and higher nursing and assisting present difficulties in performing their role with total control, beyond the area of the technologies being very specific, high-level medical requirement of customers.First, a training grid was created for nursing already contracted. Selecting the most relevant topics such as: techniques for treatment, medications and tests. Trainings are divided into classes, enabling the participation of all the nursing staff. In the end, members and the minister responsible for the training sign a sign-in sheet describing the issues raised.In addition, work began on a rotation between sectors to all present a minimal notion of routine other nursing sector. Then attention was directed new hires, a schedule to be used during the integration was created. And at the end of the training this employee has completed his form with: fit or unfit.
COMMENTS: With the work being performed, the error rate decreased and the safety of nursing in performing its role increased, since they have greater knowledge to guide each of the patients. Unfortunately, nursing research is still quite superficial in human reproduction, it is necessary that nurses engage in this context, to achieve further their education.
P-17. Excess Weight Effect in the Infertile Women Ovulation, According to The Serum Level of Progesterone and Ultrasound
C. R. Giviziez1, E. G. M. Sanchez1,2, M. C. S. Maia1, E. A. B. Fleury1, M. S. Approbato1
1Universidade Federal de Goiás – Goiânia - Brasil
2Universidade de Rio Verde - Brasil
OBJECTIVE: To evaluate the effect of excess weight in infertile women ovulatory profile, according serum progesterone levels and ultrasound.
MATERIAL AND METHODS: It was conducted a case-control study with 240 patients, aged 20 and 40, which were divided into two groups according to the ovulatory profile (I) - Probable Ovulation and (II) - Probable anovulation. It was considered probable ovulation patient with serum progesterone level ≥18nmol/l, rated in the twenty- first day of the cycle and, and the ultrasound result indicative of follicular collapse. Patients with irregular cycle, hyperprolactinemia, diabetes, thyroid disorders, levels of Follicle stimulating hormone (FSH) greater than 9.9 mIU/ml and suffering from Polycystic Ovary Syndrome were excluded from the study. Excess weight was verified by Body Mass Index (BMI), calculated according to Quetelet formula, dividing weight in kilograms by height in meters squared (kg/m2). In relation to BMI, patients were classified as normal weight (18.5 ≥ BMI < 24.99 kg/m2) and excess weight (BMI ≥ 25 kg/m2 = overweight/obesity). Comparability of ages between the groups was performed. The Microsoft® Excel 2007 program was used for data tabulation and the statistical analysis was performed using the SPSS program for Windows®, version 16.0. The differences of proportions were evaluated by Chi-square test. P values <0.05 were considered significant.
RESULTS: Of the 240 patients analyzed , 59.6 % (n = 143) had normal weight and 40.4 % (n = 97 ) excess weight. The average age of the patients with normal weight was 31.7 ± 4.4 and excess weight 32.0 ± 4.3 (p = 0.202). When evaluating the ovulatory profile by the serum progesterone level and ultrasound, it was observed that excess weight caused a significant reduction (p = 0.020) in ovulation percentage of infertile patients.
CONCLUSIONS: This study suggests that excess weight can negatively affect the ability to ovulate in infertile women.
P-18. Evaluation of In Vitro Development of Isolated Secondary Follicles in 3-Dimensional System in two Base Media Culture from Fresh and Cryopreserved Ovarian Tissue
D. L. Bulgarelli1, J. R. Campos2, C. G. Gervásio1, L. A. Batista1, M. M. Machado1, A. C. J. S. Rosa e Silva1
1Departamento de Ginecologia e Obstetrícia. Faculdade de Medicina de Ribeirão Preto. Universidade de São Paulo. FMRP-USP
2Clinica Genics Medicina Reprodutiva e Genômica – São Paulo - Brasil
OBJECTIVE: The possibility of ovarian tissue cryopreservation for subsequent immature follicle enclosed in vitro culture to obtain fertilizable oocytes is being investigated as a potential option for fertility preservation of cancer patients. Thereby, this study aimed to evaluate in vitro development until antral stage follicles from fresh and cryopreserved ovarian tissue cultured in two different base media.
MATERIAL AND METHODS: Bovine ovaries cortex were cut into 3x3x0.5mm3 fragments and were cryopreserved by vitrification method Ting et al 2013 modified. The fragments were exposed to vitrifications solutions containing 0.6 M glycerol (3min), 1/8 (3min), 1/4 (3min) , 1/2 (3min) e 1X (1 min), loaded into high-security straw with vitrification solution plus polymers, heat sealed and cooled in LN2 vapor. Samples were warmed into 40ºC water bath and cryoprotective agents were diluted with 1M, 0.5M, 0.25M and 0M sucrose. Secondary follicles were isolated, encapsulated into alginate (0.25% w/v) and cultured for 15 days at 5% CO2 in αMEM and TCM with 5ng/ml FSH. Follicle survival rate, growth rate and antrum formation rate were analyzed.
RESULTS: Following long term culture, isolated secondary follicles from fresh tissue and cryopreserved tissue were cultured. Survival rate at fresh groups was 12% TCM and 59% αMEM (P<0.05). However, αMEM cryo group showed 20% survival rate and TCM cryo group showed no survival follicles. Follicular growth TCM fresh was 12% and TCM cryo group there was no growth follicular. While, αMEM fresh group showed 52% and αMEM cryo 23%follicular growth (P<0.05). Antrum formation was 14% αMEM fresh group and 3% αMEM cryo group, while TCM fresh and cryo groups there was no antrum formation.
CONCLUSIONS: Bovine secondary follicles from cryopreserved tissue can survive and grow to antral stage when cultured in αMEM base media. Further development of the to improve the follicle culture procedures to support a fertilizable oocyte are ongoing.
P-19. Women’s Age in the First Infertility Consultation: Have Changed after Ten Years?
K. Adami1, A. C. Trigo1, G. Araújo1, M. Lusquinhos1, V. Cotrim1, J. R. C. Lopes1
1CENAFERT- Centro de Medicina Reprodutiva - Salvador, Bahia, Brazil
OBJECTIVE: To describe the age of women attending first infertility consultation in a reference center for Assisted Reproduction (RA). The woman’s age is an important predictive factor in reproductive outcomes and results of assisted reproduction techniques. The search for specialized care in infertility and optimal treatment access depends on women age that determines prospect of success.
MATERIAL AND METHODS: Cross-sectional, retrospective study considering the periods of 2004-2005 and 2014-2015, through chart review. Bank built and analysis with SPSS 20.0.
RESULTS: Between 2004 and 2005, 211 women were attended with one professional watching the cases, and in 2014 until April 2015, after increasing the number of medical assistants for six professionals, have been met 414 women, within 18 months of attendencies in each period. In the first period, the average age was 36.19 ±4.19years old and in the second period 36.57 ±3.06 years old, with no statistically significant difference (p=0.12). The mean age of patients seen compared between the different clinical professionals presented no difference.
CONCLUSIONS: Over time, we observed no change in women’s age of first infertility consultation in this center. This finding may reflect more consciously information divulgation by the media about the risks of female infertility with the postponement of conception. Clarify the importance of timely referral to infertility and women’s fertility preservation consultation determine better results prognosis in RA treatments, especially when the woman is under 40 years, and validate earlier research of reproductive capacity at 35 years and when diseases that impact negatively on reproductive condition are detected.
P-20. Results of Embryo Transfer of Cycles in a Fresh and Frozen af a Reference Center
J. Mendes1, K. Adami1, T. Leão1, V. Cotrim1, J. R. C. Lopes1
1CENAFERT- Reproductive Medicine Center, Salvador, Bahia, Brazil
OBJECTIVE: To describe the results of blastocyst transfer in fresh cycles and in devitrification cycles at a reference center in the last year. The transfer of blastocyst embryos, more advanced stage of its evolutionary stage in the laboratory, allows a better morphological selection and better pregnancy results in fertilization cycles in vitro (IVF). There is a tendency to better results related to transfer in cycles with embryo devitrification (TEC), assigning to a greater possibility of endometrial receptivity than in fresh cycles (TEF).
MATERIAL AND METHODS: Cross-sectional, retrospective study from April 2014 to April 2015, considering IVF cycles with own eggs, with evolution to the blastocyst stage in cycles fresh and devitrification. Bank was built and analyzed with SPSS 20.0.
RESULTS: Seventy-five fresh cycles with blastocysts transfers and forty-three in devitrification cycles were assisted. In TEF cycles, the median were 34.57 ± 4.93 years for women age, 8.16 ± 3.45 collected mature oocytes, 7.76 ± 3,23 inseminated oocytes, 5.83 ± 2.46 embryos and 3, 35 ± 1.87 evolving into blastocysts, 2.23 ± 0.14 transferred. There were obtained 40% (30/75) of clinical pregnancies three abortions and 80% (24/30) of ongoing pregnancies. In TEC cycles, the averages were 36.07 ± 5.0 years for women age, 4.25 ± 1.79 desvitrified embryos, 3.89 ± 1.64 and 2.41 ± 0.62 blastocysts survivors transferred. There were 65% (28/43) clinical pregnancies, four abortions and 85.7% (24/28) pregnancies in progress. When stratified by women’s age group, the group above 40 years presented 27.2% (3/11) pregnancies in TEF cycles and 60% (6/10) in TEC cycles (p 0.38) with 33% (1/3) ongoing pregnancy in TEF and 83.3% (5/6) in the TEC.
CONCLUSIONS: The rates of clinical pregnancy and its progress apear to be promising in the cycles of devitrification, equal to the results of the fresh cycles. With larger sample, could be possible to evaluate if there is difference between TEC and TEF cycles in obtaining viable pregnancies with blastocysts transfers, corroborating a possible improvement in endometrial receptivity out of fresh cycles.
P-21. Comparison of Seminal Parameters Before and After Capacitation Between two Consecutive Days of Intrauterine Insemination in the Same Individual
E. Araújo Filho1, C. L. Facio1, L. A. Machado-Paula1, J. E. Corrente2, L. Previato1
1Center of Human Reproduction of São José do Rio Preto, São José do Rio Preto, SP, Brazil
2Department of Bioestatistics, Institute of Biosciences Botucatu, São Paulo State University - UNESP, Botucatu, SP, Brazil
OBJECTIVE: To compare preparation of semen for IUI in the first and second day, in the same individual and assess whether there was an improvement in seminal parameters on day 2.
MATERIAL AND METHODS: 168 patients underwent double IUI (24h/48h), with 2-7 days of sexual abstinence. Exclusion criteria: tubo-peritoneal factor; severe male factor; severe endometriosis; >38 years old; non-response to ovarian stimulation; > 4 follicles with 20mm (on day of hCG); without abstinence suggested. Stimulation: clomiphene citrate and human menopausal gonadotropin (hMG). When at least one follicle measured 20mm (mean diameter) was administered subcutaneous hCG. First semen collection: 24h after hCG and second: 48h. Sperm capacitation technique: Isolate discontinuous concentration gradient. Seminal parameters compared before and after capacitation (24h/48h): concentration/ml, motility (progressive motility, nonprogressive, immotility) and oval sperm head. Patients were divided: group 1: all cases; group 2: light oligospermia; group 3: low concentration of oval sperm head; group 4: altered seminal parameters. Comparisons using generalized linear model with negative binomial distribution for counting data and binomial for data expressed as percentages; significance level of 5%.
RESULTS: Group 1 (N=138): before processing: difference in the concentration/ml (greater on day 1) (p=0.0009). After processing: concentration/ml greater on day 1 (p=0.0001); immotility sperm increased on day 2 (p=0.0340), and oval sperm head decreased on day 1 (p=0.0208). Group 2 (N=12): before processing: concentration/ml greater on day 2 (p<0.0001) and oval sperm head decreased on day 2 (p=0.0033). After processing: greater recovery of oval sperm head on day 1 (p=0.0024). Group 3 (N=39): before processing: concentration/ml improved on day 1 (p=0.0072). Group 4 (N=67): before processing: better concentration/ml on day 1 (p=0.0448) e after processing: immotility sperm increased (p=0.0093) and smaller percentage of sperm progressive motility (p=0.0308) on day 2.
CONCLUSIONS: Abstinence period of one day (second IUI) did not improve the motility and morphology before seminal processing in all groups. In the groups 2, 3 and 4 the difference of concentration observed before processing on days 1 and 2 of IUI was corrected by sperm processing technique (Isolate), even in group 2 that suggested improvement.
P-22. Sperm Viability after Maintenance at Different Temperatures
L. Wietcovsky1, C. A. dos Santos1, V. L. L. Amaral1, R. A. Salvador1, D. Til1, A. Siewert1
1Universidade do vale do Itajaí - UNIVALI
OBJECTIVE: This goal of this study was to analyze the sperm viability after two seminal processing techniques and maintenance for 24 hours at different temperatures.
MATERIAL AND METHODS: Fourteen seminal samples from normozoospermic men were used. The samples were divided and an aliquot processed by Discontinuous Density Gradient (GDD) or by Swim Up (SW). Human Tubal Fluid (HTF-Modified - Irvine®) was used to perform the above techniques. This media was supplemented with 10% Serum Substitute supplement (SSS-Irvine®). The samples were evaluated after processing and subsequently aliquoted and maintained at three different environments and temperatures: incubator (37°C) refrigerator (6 ± 2°C) and room temperature (21 to 23°C). After 24 hours, the samples were heated at 37 ° C for 5 minutes and reevaluated. The sperm parameters analyzed were motility and vitality. Data were analyzed using ANOVA and submitted to Tukey test at 5% error probability.
RESULTS: There was no significant difference between the rates of recovery for vitality and motility of samples kept at room temperature or in an incubator, or when processed by the GDD or SW. However, refrigerated samples had lower parameters (p <0.001) in the recovery rates for vitality and motility compared to the other groups, both using GDD or SW was observed.
CONCLUSIONS: This study suggests that maintaining processed semen samples at room temperature for 24 hours does not affect the vitality and motility of spermatozoa, giving the same results as maintaining at temperature of 37 ° C, however there is a significant reduction in sperm viability when processed semen is kept refrigerated.
P-23. Computacional Localization of Changes in Chromatin of Human Spermatozoa Stained with Toluidine Blue
E. T. Souza1, J. P. Ribeiro Junior1, B. A. N. Travençolo2, M. Beletti2
1Clinica Vita Reprodução Humana e Ginecologia Cirúrgica – Uberlândia - Brasil
2Universidade Federal de Uberlândia - Brasil
OBJECTIVE: To identify through computer image analysis the location of chromatin changes in human sperm stained with toluidine blue (TB).
MATERIAL AND METHODS: Have been analyzed 400 sperms in 8 different smears of semen. Was carried out an acid hydrolysis of the smears (4N hydrochloric acid) for 15 minutes, washing in distilled water and drying at room temperature. The slides were stained with TB, adding a drop of dye 0.025% (w / v), pH 4.0 in buffer sodium citric acid-phosphate (McIlvaine buffer), and after the slide was covered with a cover slip. After 3 minutes there was made a reading in light microscope and the images catches. Subsequently the images were processed using algorithms developed in Matlab, and run on Octave program. The algorithms perform the segmentation of the sperm’s heads and delimitates the region where is located the alteration of chromatin, if any is found. This region is identified by more intense staining in the slides evaluated in transmitted light microscope.
RESULTS: The algorithms used for computational image analysis identified and delimited regions with chromatin changes in the heads of sperm with displaying changes in coloration with TB.
CONCLUSIONS: The computer analysis is a efficient and a less subjective method of evaluation. That is why it is a good tool to identify changes decompression chromatin in semen smears stained with toluidine blue.
P-24. Vasectomy Reversal: 13-year experience
F. Pasqualotto1,2, E. Pasqualotto1,2, F. O. Castilhos1, L. T. Hofmann1, R. R. Felkl1, D. Arbusti1
1Faculdade de Medicina da Universidade de Caxias do Sul – UCS – Caxias do Sul (RS)
2Centro de Reprodução Humana – Caxias do Sul (RS) – Brasil
OBJECTIVE: Evaluate the success rate in the reversal of vasectomies and associate this rate with the time intervals since vasectomy.
MATERIAL AND METHODS: Were viewed 64 cases of vasectomy reversal performed in 13 years using the double-layer technique under microscopic magnification.
The main age of the man was 42.2 ± 12.3.
Female age at the time of the reversal was 33.2 ± 4.2.
Patients were divided according to the period of obstruction in three groups: Group A (< 10 years – 41 cases), group B (10-15 years- 8 cases), and group C (> 15 years of obstruction –
15 cases).
RESULTS: Overall, we had 57 cases of positive patency, 45 women pregnant and 43 children delivered. The patency and pregnancy rates were higher in group A (95,12%, n = 39 and 78,04% n = 32), compared to groups B (75%, n = 6 and50%, n = 4); and group C (80%, n = 12 and 60%, n = 9).
(P < 0,05).
CONCLUSIONS: Better patency and pregnancy rates are present in patients with less than 10 years of obstruction compared to patients with more than 10 years of obstruction.
P-25. Comparison of Survival and Pregnancy Rates of Human Embryos Thawed at Day 2/3 and Day 5 Using Vitrification Technique in Patients Underwent in Vitro Fertilization
L. Previato1, N. F. Sinhorini1, L. A. Machado-Paula1, C. L. Facio1, J. E. Corrente2, E. Araújo Filho1
1Center of Human Reproduction of São José do Rio Preto, São José do Rio Preto, SP, Brazil
2Department of Bioestatistics, Institute of Biosciences Botucatu, São Paulo State University - UNESP, Botucatu, SP, Brazil
OBJECTIVE: To compare survival rates between vitrified embryos on day 2/3 and day 5, and pregnancy rates between day 2/3 and day 5 embryos that survived after thawing separating by age.
MATERIAL AND METHODS: 168 patients underwent ICSI. Inclusion criteria: top-quality embryo (cryopreservation and thawing); ovarian hyperstimulation syndrome and supernumerary embryos. Patients were separated by age: < 35 years and ≥ 35. Embryos were vitrified and thawed by specific kits (Irvine Scientific, USA). Endometrium was prepared with estradiol and monitored (ultrasound) and when it measured ≥ 8 mm was given natural micronized progesterone. Embryos were thawed and transferred. Poisson distribution and Chi-square test were used and significance level of 5%.
RESULTS: Of the 168 patients, 72 (42.86%) vitrified embryos on day 2/3 and 96 (57.14%) day 5. Of these, 92 (54.76%) were <35 years and 76 (45.24%) ≥ 35. Analyzing all cases, comparison between cleavage stage (64.6 ± 33.9) and blastocyst (65.3 ± 32.0) rates was not significant (p=0.99), and separating by age, in the <35 years the cleavage (61.5 ± 32.1) and blastocyst (57.2 ± 31.1) rates have not shown difference (p=0.6680), as well as for the ≥ 35 with cleavage (69.5 ± 36.7) and blastocyst (73.4 ± 31.0) rates (p=0.7197).
Analyzing only pregnant patients: not considering age, there was no significant difference (p=0.9166) between cleavage (78.8 ± 24.2) and blastocyst (77.4 ± 25.3) rates; separating by age, <35 years the cleavage (72.4 ± 26.0) and blastocyst (68.0 ± 31.3) rates did not show statistical difference (p=0.8238), and for the ≥ 35 the cleavage (90.6 ± 16.4) and blastocyst (84.0 ± 18.8) rates also did not show difference (p=0.6407).
Comparing pregnancy rates between cleavage (17 pregnancies [43.6%]) and blastocyst (22 pregnancies [56.5%]) groups also did not show statistical significance
(p=0.365).
CONCLUSIONS: We conclude by our results that we have good pregnancy rates independent whether vitrification was carried out on day 2/3 or day 5 and that there was no interference of age. Literature shows better results with vitrification on day 5, but there are controversies.
Further studies are needed with larger group of patients to obtain new findings.
P-26. Intracytoplasmic Sperm Injection in Men with Congenital Bilateral Absence of The Vas Deferens: A Success Story
F. Pasqualotto1, E. Pasqualotto1, F. O. Castilhos1, D. Arbusti1, F. Tonietto1
1Universidade de Caxias do Sul
OBJECTIVE: Evaluate patients with congenital bilateral absence of the vas deferens who underwent fertilization by intracytoplasmic sperm injection in relation to the pregnancy rate per cycle and the live delivery rate per
cycle.
MATERIAL AND METHODS: The records of 37 consecutive men from September 2002 to December 2014 with OA due to CBAVD who underwent percutaneous epididymal sperm aspiration were retrospectively reviewed. Before ICSI, their female partners were screened for cystic fibrosis (CF) -positive on routine testing. In all cases, the result was normal. Preoperatively, each patient had undergone a thorough history and physical examination and kidney ultrasound. Sperm were obtained intraoperatively in all 37 patients. The intraoperative parameters that were analyzed included sperm concentration and motility. The average patient age was 39.0 years, and the average partner age was 34.4 years. All patients had a diagnosis of CBAVD based on physical examination. In addition, testicular volume was normal in all 37 patients.
RESULTS: From these 37 cycles, 26 pregnancies occurred (70, 27% pregnancy rate/cycle) and three couples miscarried, for a live delivery rate per cycle of 62, 16% (23/37). Deliveries included 17 singleton births, and 3 sets of twins.
CONCLUSIONS: The high success rate is likely due to the fact that men with CBAVD have totally normal spermatogenesis, the only anomaly being the absent vas deferens. In addition, our population of couples with CBAVD had healthy wives with no female factors contributing to the couples’ infertility.
P-27. Quality Control Importance of the Results of a New In Vitro Fertilization Laboratory
V. A. Comar1, M. C. N. Ligabô Junior1, K. Ribeiro1, A. S. J. Miguel1
1Mogi Invitro Laboratório Clínico
OBJECTIVE: To demonstrate the importance of quality control (QC) performed at the opening of an in vitro fertilization laboratory (IVF) with fertilization, cleavage, clinical pregnancy/cycle, clinical pregnancy/transfer and implantation rates.
MATERIAL AND METHODS:: Retrospective study of couples undergoing IVF cycle in the period January-April 2015, after strict quality control, in a IVF laboratory new and private. The study included 18 cycles of induction, of these 08 did embryo transfer and 10 only frozen embryos. The tests performed in QC were: particle counting (positive pressure); internal temperature of the incubators, the environment and the heating plates and analysis of the pH of the culture medium used. After evaluation of these parameters, adjustment was made of those who were unsuitable second bibliographical and manuals references. All equipments was calibrated and certified by the respective suppliers. This paper described fertilization rate, clinical pregnancy rate per cycle, clinical pregnancy per transfer rate and implantation rate of the procedures performed at a new IVF laboratory.
RESULTS: The study evaluated 18 started cycles, where the average age was 32.5 ± 4.95. In all cases ICSI was performed. 114 mature oocytes (MII) were injected, being the fertilization rate 78.95%, cleavage rate was 97.78%, clinical pregnancy/ cycle rate was 27.78%, clinical pregnancy / transfer rate was 62.5% and implantation rate was 53.33%.
CONCLUSIONS: The guidelines implementation for a new IVF laboratory requires a quality management program, integrating control, assurance and quality improvement. For this clinical outcome in the laboratory was essential qualified personnel, supply and maintenance of appropriate culture conditions to minimize stress to gametes and embryos and to optimize the in vitro environment as well as to conduct a thorough QC of parameters described in the methodology in addition to the laboratory cleaning.
Then, appropriate setting, monitoring and stabilization of these parameters are a crucial component of a rigorous QC program.
With these results, the new laboratory should establish quality indicators to systematically monitor and evaluate the performance of it. However, randomized studies with larger sample size should be conducted.
P-28. Bioinformatic Approach to Stablish Predictors of Oocyte Development Competence in Cumulus Cells
L. M. Meirelles1, M. A. De Bastiani1, F. Klamt1
1Laboratório de Bioquimica Celular - Departamento de Bioquimica -ICBS/Universidade Federal do Rio Grande do Sul, Porto Alegre, RS, Brasil
OBJECTIVE: The cumulus oophorus forms a set of somatic cells that surround the oocyte and have an intimate relationship with the germinative cell throughout the folliculogenesis, oocyte maturation and ovulation processes.
The gene expression and biochemical activity of cumulus cells are influenced by the oocyte conditions, follicular environment and by interactions with the ovarian
environment. Our group aim to identify processes that serve as biomarkers of oocyte quality in cumulus cells using bioinformatic tools.
MATERIAL AND METHODS: Our bioinformatic approach uses microarray data obtained from the Gene Expression Omnibus (GEO) online repository, maintained by NCBI. Specifically, we used the data deposited under the GSE37277 identifier. Our group analyzed the global processes that involve the 500 genes which showed more differentially expressed in 81 cumulus oophorus samples, divided into two sample groups (cumulus cells coming from cumulus-oocyte complexes that generated good and poor quality blastocysts). All the analysis were computed at the R statistical environment, with which the differentially expressed genes were obtained using the LIMMA package and the functional analysis of the enrichment processes were made using FGNet package.
RESULTS: 169 processes were identified associated with good quality oocytes and 68 associated with poor quality oocytes, using as reference a P ≤ 0.0005.
In the sample group of cells from complexes that generated good quality blastocysts, we observed processes related to development and morphogenesis of tissues, cell differentiation and signaling, protein metabolism, embryonic development, cell cycle and cellular response to stress.
However, in the sample group of cells from complexes that generated poor quality blastocysts, it was possible to identify processes pointing to an unfavorable environment, highlighting upregulation of toxic substances metabolization and response processes, chemistry cellular homeostasis, metabolism of reactive oxygen species and response to DNA damage.
CONCLUSIONS: The differential gene expression of cumulus cells is a reflection of their follicular microenvironment.
In view of the results, our group suggests that processes are used as oocyte quality biomarkers, since they can reflect more effectively the oocyte microenvironment than the expression of a single gene.
P-29. Twin Pregnancy after Double Transfer
V. A. Comar1, M. C. N. L. Junior1, K. Ribeiro1
1Mogi Invitro Laboratório Clínico
INTRODUCTION: The embryo transfer (ET) is the final and most vulnerable stage of in vitro fertilization (IVF) treatment, and is crucial to obtaining a good pregnancy rate. Even with good quality embryos, good pregnancy rates can not be achieved if the transfer is difficult or bad. The ET can be influenced by many factors, including test and choice of catheter, ultrasound use, mucus or blood presence and the of embryos retained in the catheter. Studies have focused on improving the ET hoping to increase IVF success rates.
CASE REPORT: Patient 26 years old, and only cause of male infertility (vasectomy). Couple with previous IVF and puncture epididymis (PESA) unsuccessfully. Tests to investigate female factor showed no changes. New IVF cycle was suggested with ovulation induction, 14 MII recovered and PESA was performed on that day. Two embryos formed, considered TOP, were transferred in cleavage stage, and endometrial with trilaminate pattern. After the transfer performed and subsequent check of the catheter, the embryologist noted that one of the embryos remained retained in the catheter. The clinician is alerted, the embryo retained was washed in the culture medium and the catheter for sequential ET recharged. This time the embryo was in the uterus. Both transfers were easily without blood or mucus on the catheter. The result of pregnancy was positive, and the twin pregnancy was confirmed by ultrasound examination, having thus 100% implantation.
COMMENTS: This study demonstrated that technical difficulties in the ET can not affect results of IVF. A repeated sequential transfer due to retained embryos in the catheter can be safely performed when required. Contrary to this account, Visser et al. showed significantly lower pregnancy rates in multiple sequential transfers to embryos that retained in the individual transfers. Nabi et al. demonstrated that retained embryos were significantly more difficult found in ET or when the catheter was contaminated with mucus or blood. In short, in this report, the ET repeated sequence did not affect the outcome of pregnancy, implantation and pregnancy in progress.
P-30. Ovarian Reserve Indicators in Patient with Hypogonadotropic Hypogonadism: A Case Report
S. A. de Oliveira1, I. A. Rocha1, M. S. Borges1, G. M. Coelho1
1Instituto Valenciano de Infertilidade (IVI - Salvador) -Brasil
INTRODUCTION: Serum anti-mullerian hormone (AMH) is mainly expressed by granulosa cells of early antral and pre-antral follicles and is considered a useful marker of ovarian reserve because is predictive of prognosis in human reproduction cycles. However, in some specific conditions like congenital or acquired hypogonadotropic hypogonadism, AMH testing and the antral follicle count may not be reflective of the ovarian reserve because in these patients, ovarian reserve testing can be challenging due to the contracted appearance of the ovaries and low AMH levels that despite being produced in part by gonadotropin-independent cells (pre-antral follicles), also has its output dependent cells gonadotropin (antral follicles). When treated with LH (indispensable in these cases) and FSH (urinary or recombinant) in high dosis, these patients may exhibit increased AMH levels and demonstrate adequate follicular development.
CASE REPORT: A 36-year-old nulligravid patient with hypogonadotropic hypogonadism due to a surgical treatment of pituitary adenoma. This patient presented low FSH (0.3 IU/L), LH (0.1 IU/L), estradiol (77 pmol/L), AMH levels (0.65 pmol/L) and 4 antral follicles. It was made an in vitro Fertilization cycle with 150 IU daily injections of Human Menopausal Gonadotropin (hMG) and 250 IU of Recombinant FSH for 14 days and the administration of GnRH Antagonist (Ganirrelix, 0,25mg/dia) have started on the eighth day (2 follicles ≥ 14mm). 11 oocytes were collected and among them, 10 were mature (MII). 5 embryos were fertilized, all of good quality and they came to blast. 2 embryos were transferred (fresh) and 3 embryos were frozen. 12 days after the transfer, the beta HCG was 220.00 mIU/mL and the ultrasonography performed later, showed a topic single live embryo. There were no complications throughout pregnancy.
COMMENTS: This case emphasizes the challenges of assessing ovarian reserve and predicting response to stimulation in patients with hypogonadotropic hypogonadism. The contracted appearance of the ovaries can make the antral follicles count difficult. Similarly, AMH is a reliable ovarian reserve marker and it is considered the gold standard, but not in cases of hypogonadotropic hypogonadism, therefore requiring more studies to validate other markers for this condition.
P-31. Effect “In Vitro” of the Ultrasound Transmission Gel on the Total Sperm Motility
L. C. T. D. do Carmo1, F. M. Reis1, F. A. N. Pereira1, S. F. Nery1, M. A. F. Vieira1, M. T. V. Pereira1
1HC/UFMG
OBJECTIVE: To evaluate the effects of ultrasound gel on sperm motility.
MATERIAL AND METHODS: Semen samples were collected and produced by masturbation after 48 to 72 of sexual abstinence and maintained at 37ºC under 5% CO2 until complete liquefaction and throughout the experiment. The samples were evaluated according to the WHO criteria. Were chosen normospermic men with spermatic motility above 90%. The spermatozoa with progressive motility (type A and B), nonprogressive (type C) and immotile (type D) were separated from the seminal liquid by standard swim-up technique. Fixed 100 μl swim-up sperm was added to each sample to the ultrasound gel, Carbogel® ULT (Carbogel Industria e Comércio Ltda) – pH 7,3; 108 mOsmol/kg; water, propylenoglicol, polimer carboxyvinyl - in different concentration (v/v) of 10, 20 and 40% at various time intervals (0, 1, 2 and 24 hours). SpermrinseTM (Vitrolife, Inc.) was the common medium for all incubation. The control has only swim-up sperm and SpermrinseTM. Total motility (spermatozoa type A, B and C) evaluation was counted in duplicate, media average percentage and performed on light microscopy and blood cell counter.
RESULTS: There was a significant difference among control group and 10% group gel concentration. The total motility at 10% gel concentration decrease to 50% in the first hour, 42% in the second hour and after 24 hours the motility was not observed. In the groups with 20 and 40% gel concentration the spermatic mobility completely inhibited at all times (hs) incubation.
CONCLUSIONS: Our preliminary results show that the ultrasound transmission gel is toxic and impair the motility sperm in vitro.
P-32. Subclinical Hypothyroidism does not Compromise Assisted Reproductive Technology Outcomes
M. A. Coelho Neto1, W. P. Martins1, A. S. de Melo1, R. A. Ferriani1, P. A. A. S. Navarro1
1Departamento de Ginecologia e Obstetrícia, Faculdade de Medicina de Ribeirão Preto, Universidade de São Paulo (DGO-FMRP-USP), Ribeirão Preto, Brasil
OBJECTIVE: The importance of preconception thyroid-stimulating hormone (TSH) concentrations in infertile patients undergoing controlled ovarian stimulation (COS) for for in vitro fertilization (IVF)/intracytoplasmic sperm injection (ICSI) remains unclear. There is no consensus regarding screening of infertile patients for thyroid disease by measuring TSH or regarding the cut-off TSH concentrations for subclinical hypothyroidism (<2.5 or <4.0/4.5 mIU/L). This study compared reproductive outcomes in patients with TSH concentrations of <2.5 mIU/L, 2.5–4.0 mIU/L, and 4.0-10.0 mIU/L undergoing IVF/ICSI.
MATERIAL AND METHODS: This retrospective cohort study evaluated the medical records of all women with measured TSH concentrations who underwent IVF/ICSI between January 2011 and December 2012. Patients were divided into groups according to TSH concentrations: <2.5 mIU/L; ≥2.5 and <4.0 mIU/L; ≥4 mIU/L and <10.0 mIU/L; and those using levothyroxine. Primary endpoints were clinical pregnancy, miscarriage, live birth and multiple pregnancy rates. Continuous variables were compared by ANOVA (normal distribution) or by Kruskal-Wallis tests. Binary data were compared by χ• tests. The level of significance was defined as p < 0.05.
RESULTS: During the study period, 787 women underwent IVF/ICSI. Sixty were excluded because TSH concentrations were unavailable. The prevalence of hypothyroidism was 15.13%. Patient characteristics, type of COS and response to COS did not differ among the groups, nor were there differences in primary endpoints (Table 1).
CONCLUSIONS: Response to COS, miscarriage and live birth rates were not altered in women with subclinical hypothyroidism undergoing IVF/ICSI. These findings reinforce the uncertainties related to the impact of TSH concentrations on reproductive outcomes after assisted reproductive techniques.
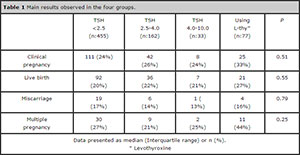
Table 1: Main results observed in the four groups.
P-33. First Description of Blastocyst Production from Ovarian Cortex Xenograft Under the Back Skin of Mice
M. T. Dias1, F. E. L. Marinho1, T. J. M. Alves1, C. M. Assunção2, P. H. A. Campos-Junior1
1Laboratório de morfofisiologia e biotecnologia gonadal – UFSJ-Universidade Federal De São João Del Rei Campus Dom Bosco -Brasil
2Embrapa Gado de Leite - Brasil
INTRODUCTION: The chemo/radiotherapy adequacy entails an improvement on surviving of reproductive-period of oncological female patients. Ovaries are very sensible to cytotoxic treatment, resulting in an increasing number of patients with premature ovarian death. Grafts techniques are alternatives to fertility preservation. So far, it has been published 35 births from auto-grafts oocytes, however in this technique there is a risk of neoplastic re-incidence. The aim of this study was to assess the feasibility of ectopic ovarian cortex xenograft (using bovine model) under the back skin of immunodeficient mice.
MATERIAL AND METHODS: Female SCID mices (~60 days, n=25) was anesthetized with ketamine/xilazine. Then, they were placed on ventral decubitus and 4 incisions were made bilaterally and divulsed on dorsal region, and grafted with ovarian fragments (1.5mm•), so they were sutured.
After 10 days, the receptors were euthanized and the xenografts were recovered. The mices and grafts weights were assessed before and after surgery. Xenografts were processed to histology (HE) and analyzed in relation to the folliculogenesis progression.
To harvest the oocytes, the ovarian slicing was performed, the oocytes were morphologically classified and submitted to IVF. Averages (±SED) were calculated and compared using t-student test.
RESULTS: There was no significant difference (P>0.01) between the receptors mice body weight before and after xenograft (respectively, 20.5±0.4g and 21±0.8g). However, the grafts weight 10 days after the transplant was significantly higher (P<0.01; before: 11.6±3.4mg; after: 14.8±5.2mg), indicating ovarian tissue development ectopically. Using the histological evaluation, primordial, primaries, multilaminar, antral and atretic follicles were observed, indicating graft-tissue folliculogenesis progression, and neo-angiogenesis. 22 oocytes (12 degree I, 9 degree II and 1 degree III) were harvested from ovarian xenograft, which, after IVF, give rise to 2 blastocysts (D7).
CONCLUSIONS: This study showed, for the first time in the literature, which ovarian xenografts were: (i) healthily maintained under the back skin of immunodeficient mice, (ii) responsible to murine gonadotrophins, (iii) able to produce oocytes that (iv), by IVF, originated blastocysts. In general, our findings clearly showed the feasibility of the xenograft technique as an alternative to female fertility preservation. CEUA/UFSJ-009/15
P-34.N-Acetyl-Cysteine Prevents Damages to Embryonic Development Induced by Follicular Fluid from Infertile Women with Mild Endometriosis: In Vitro Study Using Bovine Model
V. S. I. Giorgi1, C. C. P. de Paz2, R. A. Ferriani1, P. A. A. S. Navarro1
1Department of Obstetrics and Gynecology, Faculty of Medicine of Ribeirão Preto, University of São Paulo - Brazil
2Department of Genetics, Faculty of Medicine of Ribeirão Preto, University of São Paulo - Brazil
OBJECTIVE: To assess the effect of the addition of follicular fluid (FF) from infertile women with and without mild endometriosis (ME) and of the antioxidant N-acetyl-cysteine (NAC) on embryo development, using bovine model.
MATERIAL AND METHODS: FF samples were obtained from 22 infertile women undergoing ovarian stimulation for intracytoplasmic sperm injection [11 with ME (EFF) and 11 with tubal and/or male factor of infertility (CFF)], pooled, and utilized in 5 in vitro maturation (IVM) experiments with immature bovine oocytes (IBO). IBO were submitted to IVM divided in 5 groups: without FF (NF), with 1% of FF from ME patients (EFF) or control patients (CFF), EFF + 1.5mM of NAC (ENAC), CFF + 1.5mM of NAC (CNAC). Then, in vitro fertilization (IVF) was performed and embryos were in vitro cultured. We analyzed cleavage, blastocysts production and hatched blastocysts rates. Data were analyzed by gamma distribution.
RESULTS: A total of 484 cumulus oocyte complexes (COCs) were inseminated with sperm and the embryos were cultivated in vitro. The cleavage rate was similar comparing NF (65,0%) with CFF (61.5%, p=0.6063), CNAC (57.1%, p=0.2058) and ENAC (57.7%, p=0.1789); and lower comparing EFF group (50.5%) with NF (p=0.0072) and CFF (p=0.0297) groups. The blastocyst production rate was similar in NF (38.0%) and ENAC (37.1%, p=0.5436) groups, and lower than NF in CFF (29.2%, p=0.0190), CNAC (26.5%, p=0.0026) and EFF (25.8%, p=0.0038). Relative to the hatched blastocysts rate, NF (60.5%) was similar to CFF (57.1%, p=0.8367); the EFF (37.5%) had the lower hatched blastocysts rate compared another groups [vs NF (60.5%, p<0.0001), vs CFF (57.1%, p<0.0001), vs CNAC (76.9%, p<0.0001) and vs ENAC (75.0%, p<0.0001), and NAC increased this rate in groups with FF from women with (EFF vs ENAC: p<0.001) and without ME (CFF vs CNAC: p=0.002).
CONCLUSIONS: FF from infertile women with ME compromises cleavage and hatching blastocysts rates of in vitro fertilized bovine oocytes which is prevented by the antioxidant NAC. We question whether the use of NAC could improve the results of Assisted Reproduction Techniques in ME patients.
Financial funding: FAPESP (process number: 2012/15070-1), Brasil.
P-35. Analysis of Pregnancy rate after Intrauterine Insemination and its relation to the Etiology of Infertility
A. P. Ceschin1, M. C. São Miguel2, L. K. S. Nishikawa1, L. B. Zraik2, R. S. Chamma2
1Felicitá Instituto de Fertilidade – Curitiba - Brasil
2Pontifícia Universidade Católica do Paraná (PUCPR)
OBJECTIVE: To analyze the pregnancy rate after intrauterine insemination and correlate these values to the cause of infertility.
MATERIAL AND METHODS: A retrospective study was realized with records of 311 patients undergoing intrauterine insemination at a private clinic for infertility from January 2012 to April 2014. The patients were divided according to cause of infertility: cervical, ovulatory dysfunction, endometriosis, age, multiple, male and unexplained infertility.
The data was compared to evaluate the pregnancy rate after the procedure and its relation with cause of infertility. To the statistical evaluation the chi-square test was performed, set as significant p <0.05.
RESULTS: The pregnancy rate after intrauterine insemination was 16.1% (n = 50). There was no statistical significance difference to compare the success of the procedure with the cause of infertility. Although the best pregnancy rates was observed in unexplained infertility.
CONCLUSIONS: There was no direct correlation between the pregnancy rate after intrauterine insemination and the cause of infertility. The best success rates were observed in unexplained infertility, but there’s not statistical significance. Other studies are needed to try to determine if there is any cause of infertility that will benefit more with intrauterine insemination.
P-36. Effect of Severe Oligospermia on Embryo Formation in ICSI Infertile Patients
M. Approbato1, T. M. da Silva1, M. C. S. Maia1, R. S. Florencio1, I. Silveira1, F. C. Approbato1
1Reproduction Human Laboratory. Federal University of Goias State, Brazil
OBJECTIVE: ICSI has been spread as an infertility technic to oligospermic patients. As the sperm count goes down, the embryo formation in more and more affected. The main object of this paper is evaluating the effect of a severe oligospermia in embryo formation, embryo quality and pregnancy.
MATERIAL AND METHODS: A Cross-sectional study, with 102 patients (48 with TMSP – Total Mobile Sperm Processed <= 1,0 x 106 - Group 1 and 54 with TMPS >= 12 x 106 - Group 2). We compare the following variables: embryo quality (percentage of A embryo or morula on D3 post ovum pick up), percentage of embryo formation and chemical pregnancy (positive b-hCG). The following variables (confound factors) were paired: Age, BMI, Infertility duration (months), basal FSH, basal Estradiol. We use the Mann-Whitney U and Chi-Square test statistics (p = 0,05). Calculations were done with SPSS 17.0.
RESULTS: There was a statistical difference between embryonic A / Morula percentage (Group 1, X = 17,51 % x Group 2 X = 38,45 p = 0,03). There was a statistical difference in percentage of embryo formation (Group 1 X = 28,71 and Group 2 = 43,77 p = 0,029). There was no statistical difference at a chemical pregnancy between the two groups (Group 1 = 14,6 % and 23,4 % in group 2).
CONCLUSIONS: The severe oligospermia affect both quality (reduction of 21 %) and embryo formation (Reduction of 15 %). Though the number of chemical pregnancy was greater (8%) on TMPS > 12 x 106, this difference was had not statistical significance.
P-37. Case Report : Pioneer Experience the Discipline of Human Reproduction in Biology Courses in Brazil
P. F. Taitson1, N. D. S. Xavier1, M. A. Andrade1, J. A. Figueiredo1
1Departamento de Ciências Biológicas, Pontifícia Universidade Católica de Minas Gerais (DCB/PUC-Minas)
INTRODUCTION: Constant evolution in educational technology has raised the need to reflect on teaching practice and to discuss this practice among educators and health professionals.
CASE REPORT: To allow our students learn more easily the content of the discipline of Human Reproduction, we prepared a discipline which we incorporated suggestions given by students aiming to improve the teaching-learning relationship and then use them in regular courses. Teachers and students have developed a model to prioritize their desires about how it should develop the discipline itself.
Course participants conducted interdisciplinary action-based research activities using different dialogical teaching-learning methods. This strategy was performed for eight consecutive semesters (February 2011 to December 2014), with graduate students in biological science, medicine, biomedicine and nursing at the Pontifical Catholic University of Minas Gerais (PUC Minas).
COMMENTS: We interact with 321 students to identify their difficulties and incorporating their requests whether in terms of development or the evaluation in order to provide a real improvement of the learning process that is our main goal. We worked to obtain that each student could develop their learning to the limit of their possibilities and stimulate the dialogue to facilitate the teaching-learning relationship. This is the pioneering experience of Human Reproduction discipline in Biology courses in Brazil according to MEC/Brazil.
P-38. Seminal Analysis of Patients Post Vasectomy: Centrifuging is Necessary?
A. P. A. G. K. Porto1, P. M. Scanhola1, R. A. A. Navogino1, E. D. Cavassin1, D. S. Zylbersztejn1, J. C. C. I. Truzzi2
1Setor de Análise Seminal do Laboratório Fleury Medicina e Saúde, SP - Brasil
2Setor de Urologia do Grupo Fleury Medicina e Saúde, SP - Brasil
OBJECTIVE: To evaluate vasectomized patients before and after centrifugation and meet or disagree with the guidelines in question. About 42 million patients worldwide rely on vasectomy as a contraceptive method to be a simple, reliable and effective technique. The method consists of surgical interruption of the vas deferens preventing the exit of sperm from the testicles. Statistically there is a technical failure every 2000 cases as oral contraceptive method fails to 100 cases. Semen analysis is an essential part of monitoring of post-vasectomy patients and is preferably performed three months after the procedure or at least 20 ejaculations.
Some authors differ in the laboratory procedure of post-vasectomy monitoring. The American Urological Association (AUA) refers be unnecessary conducting centrifugation of the material in the cases of azoospermic the examination fresh post-vasectomy. Already the Canadian Urological Association (CUA) shows that it is necessary to spin the material in cases of azoospermic in fresh examination.
MATERIAL AND METHODS: Cross-sectional study of 248 samples of vasectomized patients from 10/01/2014 to 07/03/2015. 27 patients were considered to 71 years old, with post-vasectomy time of 20 days and maximum of 2 years.
RESULTS: 248 samples of vasectomized patients with absence of sperm in checking fresh; 205 samples (82.66%) showed no post-centrifugation sperm (azoospermic) and 43 samples (17.34%) had sperm post-spin properties (criptozoospermic).
CONCLUSIONS: Like all criptozoospermic patients had sperm real estate, it can be said that vasectomy surgery was successful. Our results are in line with the guideline of the AUA, making less work for the laboratory seminal analysis procedure for vasectomized patients and improving the laboratory dynamics. The presence of rare sperm post-spin properties brings a sense of discomfort and insecurity for both the doctor and the patient. In these cases, all the existing guidelines on vasectomy are adamant to release patients to sexual intercourse without additional protection, except when there is a diagnosis of criptozoospermic with mobile sperm.
P-39. Factors that Influence Human Pregnancy Rates in Intrauterine Insemination. I. Single or Double Insemination/Cycle
R. S. Florêncio1,2, M. R. Borges2, J. P. Rocha2, E. C. de Castro2, M. N. C. R. Camarço2, C. L. A. de Castro2
1Laboratorio de Reprodução Humana Faculdade de Medicina-Universidade Federal de Goias Brasil
2Humana Medicina Reprodutiva – Goiânia - Brasil
OBJECTIVE: To determine the chances of chemical pregnancy, clinical and development in intrauterine insemination partner (IUI-p), single or double/cycle.
MATERIAL AND METHODS: Four hundred and forty-one IUI-p cycles with the partner sperm were evaluated from January 2010 to December 2014. Among those, 244 underwent only one procedure/cycle, 32-26 hours post hCG treatment and 197 with 2 procedures/cycle, 14-18 hours and 37-40 hours post hCG treatment. The induction was according to the following: 1 - 100mg clomiphene from 2-6 day of the cycle (2.4% of cycles); 2 - daily subcutaneous (sc) gonadotropins (75 UI) from 2-3 day of the cycle, or alternate days, with or without clomiphene (37.8% of cycles); 3-sequentially, characterized by the use of 100mg clomiphene from 2-6 day of the cycle and recombinant or urinary gonadotropin, 75 UI, subcutaneous from the sixth day of the cycle (59.6% of cycles); 4-daily sc gonadotropins (150 UI) on alternate days from the second day of the cycle (0.2% of cycles). The routine of semen preparation consisted of the collection of semen 1 hour before the procedure. After semen liquefaction, the sample was diluted in a 1: 1 ratio with HTF medium® and then it was centrifuged at 80G for 15-20 minutes. Following centrifugation, we discarded the supernatant and we added 0.5 ml of medium G-mops® and then we placed the sample in the incubator for 45 minutes. Then we perform the procedures using the Insemi Cath catheter (Cook®) or rarely the Frydman catheter. We used Utrogestan®200 vaginal in the luteal phase, 8/8 hours. BhCG dosage was carried out after 14 days. Chemical Pregnancy was above 25 mIU/ml, clinical pregnancy (gestational sac presence) and pregnancy development (≥ 12 weeks of gestation).
RESULTS: The chances of chemical pregnancy, clinical pregnancy and development in ≤ 42 years old were respectively, in the case of 1 and 2 procedures/cycle: 25.4%, 27.9%, p= 0.553; 22.9%, 23.8%, clinical; and 20%, 21.3% regarding development.
CONCLUSIONS: There was no statistical difference in the chance of pregnancy by single or double insemination/cycle when we evaluated three age groups, up to 42 years old.
P-40. Serum Estradiol During Mid-Luteal Phase of IVF/ICSI Patients Showed Higher Concentration in Pregnant, Regardless the Number of Collected Egg Cells
R. S. Florêncio1,2, M. S. B. Meira2, M. V. da Rocha2, J. P. da Rocha2, V. A. de Oliveira2, M. C. C. F. Finotti2
1Laboratorio de Reprodução Humana - Faculdade de Medicina –Universidade Federal de Goias – Brasil
2Humana Medicina Reprodutiva – Goiânia - Brasil
OBJECTIVE: Assess patients submitted to embryo transfer who underwent measurements of serum estradiol (E2) in transfer day (TD + 7), and correlate it to chance of pregnancy and other variables that interfere with the chance of pregnancy.
MATERIAL AND METHODS: One hundred and sixty-seven patients primarily submitted to ICSI from 01/01/2010 to 12/31/12, with the same examiner during all the stages, except the work of embryologists accounting for 27% of all clinical ICSI procedures in the same period. The patients included in the study consisted of who underwent embryo transfer and had used human chorionic gonadotropin for the final maturation. Most patients used antagonists and a small percentage used induction as an adjuvant, low-dose agonist. The luteal phase was supplemented with 6 mg estradiol valerate/day and vaginal micronized progesterone 600 mg/day. There was no patient exclusion who underwent embryo transfer, regardless of their age or ovarian reserve. All patients underwent E2 dosage in TD + 7 or rarely during TD + 6 or 8. We conducted a comparison of pregnant (P) and no pregnant (NP), the E2 variables, number of egg cells collected, formed embryos and transferred embryos.
RESULTS: The mean estradiol concentration, standard deviation, and t-test (p) for three age groups and P (46%) e NP(54%): patients <35 years old, 1096.54 +- 1105.30 versus 563.47+-843.99, p=0.0056; patients 35-39 years old, 773.60+-622.88 versus 357.80+-260.53, p=0.0019; patients 40-42 years old, 447.66+-206.33 versus 394.80+-175.16, p=0.2642. Patients with estradiol > 500 pg/ml (TD + 7) showed 63.2% P and 32% of P for ≤ 500 pg/ml, p=0.006. There was no statistical difference for the other variables, except for the number of formed embryos.
CONCLUSIONS: In the present study pregnant patients showed estradiol measurements in the DT + 7, with highest significance up to 39 years old, high chance of pregnancy with estradiol > 500 pg/ml and increased number of formed embryos.
P-41. High Pregnancy Rate of using Natural Cycle
J. Michelon1,2, L. Okada1, R. Azambuja1, D. Kvitko1, M. Badalotti1,2, A. Petracco1,2
1Fertilitat – Centro de Medicina Reprodutiva – Porto Alegre
2Departamento de Ginecologia e Obstetrícia da Faculdade de Medicina da PUCRS – Porto Alegre
OBJECTIVE: To demonstrate the implantation and clinical pregnancy rates after transfer of cryopreserved blastocysts using natural cycle.
MATERIAL AND METHODS: Forty-four women who had cryopreserved blastocysts were randomly selected for transfer of one or two embryos, using the natural menstrual cycle, during the year of 2014. After spontaneous ovulation, transfer was carried out within five days.
Of these patients, 64.3% had performed the transfer of blastocysts in fresh cycles, however, unsuccessful pregnancy. The cryopreservation technique applied was vitrification (Kitazato protocol).
RESULTS: The mean age of women was 33.6 years.
The mean endometrial thickness at the time of transfer was 10.5mm.
The clinical pregnancy (PR) and embryo implantation rates (IR) were 72.7% and 59.1%, respectively. Twenty-seven women (61.3%) transferred two embryos with a PR of 85.2% and 17 women (38.7%) transferred just one blastocyst with a PR of 52.9%.
The twin pregnancy rate, abortion, and ectopic pregnancy were 37%, 18.7% and 12.5%, respectively.
CONCLUSIONS: The physiology of the natural cycle favors high endometrial receptivity for cryopreserved
blastocysts. The high rates obtained from clinical pregnancy and embryo implantation may allow elective freezing of blastocysts and a single embryo transfer.
P-42. Possible Correlation Between Markers of Antioxidant Activity and Vitamin D in the Follicular Fluid of Women undergoing ICSI Technique
B. M. Pizarro1, A. C. A. Mancebo2, R. A. Antunes1,2,3, M. C. B. de Souza2, R. S. Fortunato1, T. M. Ortiga-Carvalho1
1Instituto de Biofísica Carlos Chagas Filho, Universidade Federal do Rio de Janeiro - Brasil
2Clínica Fertipraxis – Rio de Janeiro - Brasil
3Maternidade Escola, Universidade Federal do Rio de Janeiro – Rio de Janeiro - Brasil
OBJECTIVE: Studies suggest that oxidative stress is detrimental to the process of in vitro fertilization.
It is speculated that an increase in reactive oxygen species in the follicular fluid (FF) would be associated with the failure of the process. Studies suggest that vitamin D also affects the assisted reproduction process, however, data are still preliminary and controversial.
It is suggested also that vitamin D protects against oxidative stress in diabetic patients and elderly women. Here, we evaluate the possible correlation between markers of antioxidant activity and vitamin D concentrations in FF of women undergoing ICSI technique.
MATERIAL AND METHODS: Approved by Brazil platform. Of 194 women with different causes of infertility, 144 women aged 36.40±0.34 years, with a BMI of 23.29±0.33 undergoing ICSI between september 2012 and march 2014 were included in the study. The first aspirated follicle was collected from each patient on the day of oocyte captation, 36 hours after the hCG injection. We evaluate the thiol grouping (glutathione in the reduced form is the main non-protein thiol), superoxide dismutase (SOD) and total antioxidant capacity (TAC) by well-established colorimetric methods. Vitamin D levels were obtained by chemiluminescence. The intrafollicular analysis of estradiol and progesterone were made by specific radioimmunoassay and serum measurements were provided by patients. Data were analyzed by Spearman or Mann Whitney. Differences were considered significant at p<0.05.
RESULTS: There was no correlation between thiol, SOD and TAC and the levels of intrafollicular vitamin D.
An increased TAC is associated with higher levels of SOD and thiol. We also observed that, a higher TAC is associated with greater number of follicles (P = 0.013) and oocytes (P = 0.002). Dividing the patients into 3 levels of TAC, we saw that women with higher TAC produced an average of 5 oocytes (SD 3.7) and women with less TAC had 3 oocytes (P <0.001). Follicles with greater TAC had lower progesterone concentrations.
CONCLUSIONS: In this group of patients, there was no correlation between vitamin D and the studied markers of antioxidant activity. However, a higher TAC in the FF was associated with a greater number of follicles and oocytes.
P-43. Possible Correlation Between the Polymorphisms of Vitamin D Receptor (VDR) and Female Fertility
M. W. Reginatto1, R. A. Antunes1,2,3, A. C. A. Mancebo3, M. C. B. de Souza3, E. Bloise1, T. M. Ortiga-Carvalho1
1Instituto de Biofísica Carlos Chagas Filho, Universidade Federal do Rio de Janeiro - Brasil
2Maternidade Escola, Universidade Federal do Rio de Janeiro – Rio de Janeiro - Brasil
3Clínica Fertipraxis – Rio de Janeiro - Brasil
OBJECTIVE: Vitamin D acts in mineral homeostasis and have genomic actions mediated mainly by its nuclear receptor (VDR). Polymorphisms in the VDR gene affects cell proliferation, immune system and processes not correlated with bone homeostasis. The vitamin D is present in follicular fluid (FF) and the VDR is expressed in granulosa cells, however, its role in female fertility is controversial. Here we compared the frequencies of Taq1, Bsm1 and Fok1 VDR polymorphisms in fertile women to women undergoing to ICSI. We also, correlated the polymorphism frequencies with FF vitamin D levels and treatment outcome.
MATERIAL AND METHODS: Of the 200 women undergoing ICSI, 70 were selected for the “infertile” group. Were excluded male factor and secondary infertility. 120 women with, at least, one natural pregnancy to term were selected for the “fertile” group. Genomic DNA was extracted from leukocyte, submitted to PCR reaction, followed for restriction fragment polymorphism technique.
The intrafollicular vitamin D was measured by chemiluminescence and data were analyzed by Qui-square, T-student, ANOVA and two-way ANOVA, p ≤ 0.05.
RESULTS: There was no significant difference between the frequencies of Taq1 and Fok1 polymorphism between fertile and infertile groups.
The frequencies of Bsm1 were also not different (p=0.058), but, when we analyzed the allelic frequency, we saw an increase in polymorphic allele in fertile patients (p=0.02).
This higher frequency, however, did not demonstrate any correlation with vitamin D intrafollicular levels of these patients. Comparing the number of captured follicles between infertile women with Taq1 polymorphism (10.95±1.5), we saw a significant decrease (p=0.04), when compared to control group (16.57±3.04). In relation to treatment success, only half of infertile patients achieved the embryo transfer. Of these, we found a significant correlation (p=0.02) between pregnancy rates and presence of Bsm1 polymorphism.
CONCLUSIONS: The frequencies of the polymorphisms Bsm1 and Taq1 were different between fertile and infertile women. It is necessary to increase the number of cases to confirm our findings and more studies are necessary to identify possible mechanisms that justify the changes observed.
P-44. Influence of Semen Quality on the Success of Intrauterine Insemination of a Clinic for Assisted Human Reproduction (Salvador - Bahia)
A. S. Almeida1, L. D. T. de Queiroz1, J. F. dos Santos1, M. S. Borges1, G. M. Coelho1
1Clínica IVI - Medicina Reprodutiva -Salvador – BA - Brasil
OBJECTIVE: To evaluate the influence of sperm quality in reproductive success of intrauterine insemination in patients in a reference clinic in the city of Salvador.
MATERIALS AND METHODS: We studied, retrospectively, 208 cycles of intrauterine insemination (IUI) treated between January 2012 to March 2015 in a clinical Salvador.
The data analyzed consisted of collections of intrauterine insemination procedures performed, where the main seminal factors were observed (concentration, motility and morphology) and its relation to the success or failure of pregnancy.
Statistical analysis was performed using the SPSS software (version 22.0) and Microsoft Excel 2010. The chi-square test (x2) was used to assess the existence of an association between the qualitative variables.
RESULTS: The analysis of seminal parameters, it was observed that they had no influence on the result of predicting whether IUI would be positive or negative, but only to examine the positive results, it was noted that both the concentration and the motility had satisfactory effects (80.5% and 90.2%, respectively), whereas there was no significant influence of the morphology
(63.4%).
CONCLUSIONS: We conclude that the main seminal variables were not correlated with positive or negative results of IUI, but had a significant influence among the positive results. Among the variables analyzed, presented the highest expression of positive results was the progressive
motility.
P-45. Blastocyst Rate of a Laboratory of In Vitro Fertilization Showing Effective Quality Control
D. P. de Freitas1, M. S. Borges1, C. P. Teixeira1, J. F. Santos1, L. D. T. Queiroz1, G. Coelho1
1Clínica IVI Salvador/BA - Brasil
OBJECTIVE: To relate embryonic development with the quality control of an IVF laboratory, taking into account the development rates to the blastocyst stage embryos of patients undergoing ICSI (intracytoplasmic sperm injection).
MATERIALS AND METHODS: A retrospective cohort study with 65 patients with a mean age of 36.7 years who underwent ICSI, the embryos were cultured to D5 / D6, in the period from May to August 2014. The embryos were grown in ideal conditions of temperature and CO2 (37 ° C and 5% CO2) at Forma Scientific incubator in the IVF laboratory using a sequential medium culture.
RESULTS: The average rate of embryos that developed to the blastocyst stage, this period was 72.84%. Being 78.7% in May / 2014, 66.66% in June / 2014, 59.6% in July / 2014 and 86.4 in July / 2014.
CONCLUSIONS: The embryo culture should occur with effective quality control. Good rates of embryos develop to the blastocyst stage show that the cultivation environment and the manipulation of gametes and embryos are taking place under ideal conditions. Prolonged cultivation is a favorable factor to the selection of embryos and consequently increases the pregnancy rate of patients undergoing IVF treatment.
A laboratory with good blastocyst rates tends to get better pregnancy rates and much needed care and attention to maintain the environmental quality control, equipment and personnel resources.
P-46. Age Influence on Quality Seminal Related to the Analysis of Fluorescent in Situ Hybridization (FISH) an Spermatic Human Reproductive Clinic (Salvador - Bahia)
L. D. T. De Queiroz1, M. S. Borges1, Á. S. Almeida1, J. F. Santos1, D. P.freitas1, G. M. Coelho1
1Instituto Valenciano de Infertilidade (IVI - Salvador) - Brasil
OBJECTIVE: To evaluate the influence of age on semen quality of men with marital framework infertility undergoing analysis fluorescence in situ hybridization (FISH) sperm in a private clinic for human reproduction.
MATERIALS AND METHODS: Retrospective study, which evaluated the semen analyzes of these patients being investigated for conjugal infertility in the period July 2010 to May 2015, in an assisted reproduction service in northeastern Brazil. 22 patients undergoing sperm evaluations were included. The following parameters were analyzed: volume, concentration, motility, morphology and genetic analysis of chromosomes. The under investigation have been divided into groups, according to results of each variable. The groups for the seminal volume were: hypospermia, normospermia and hyperspermia. Groups related to sperm concentration were: azoospermia, oligospermia, normospermia and polyspermy.
The groups related to motility were: normal motility and asthenospermia. The groups relating to morphology were normal morphology and teratospermia. Groups related to FISH in genetic analysis were normal and abnormal.
RESULTS: The average age of the patients with normal parameters between groups were compared with those of altered groups and was not found relationship between the two. Of the 22 patients analyzed the FISH and sperm, these only 9 obtained normal results.
CONCLUSIONS: We conclude that according to the main seminal variables were not correlated with normal or abnormal results of semen analyzes, as well as age of the patients.
P-47. Frozen Embryo Transfers Do Not Affect the Newborn Weight when Compared to Fresh Transfers in IVF Cycles
M. M. Piccolomini1, M. Nicolielo1, N. Nobrega1, J. R. Alegretti1, P. C. Serafini1,2, E. L. A. Motta1,3
1Huntington Medicina Reprodutiva, São Paulo – SP, Brasil
2Disciplina de Ginecologia - Departamento de Obstetricia e Ginecologia. Faculdade de Medicina da Universidade de Sao Paulo (FMUSP), São Paulo – SP, Brasil
3Disciplina de Endocrinologia Ginecológica - Departamento de Ginecologia. Escola Paulista de Medicina - Universidade Federal de Sao Paulo, São Paulo – SP, Brasil
OBJECTIVE: The assisted reproductive practice widespread has raising concerns about safety and long-term consequences on babies born. It is demonstrated higher premature birth and low-weight rates due to the greater incidence of multiples. Moreover, recent studies have shown increased rate of Large for Gestational Age babies born after frozen IVF cycles compared to fresh IVF cycles or natural conception.
The aim of our study was to evaluate if frozen-thawed embryo transfer affect the newborn growth weight when compared to fresh embryo transfer in IVF cycles.
MATERIAL AND METHODS: This retrospective cohort study evaluated 1037 deliveries from IVF cycles using standard conventional treatment protocol between 2001 and 2013. It were evaluated 631 deliveries obtained from fresh-embryo transfer (Fresh-ET) and 406 from frozen-thawed-embryo transfer (Frozen-ET). Patients received 1 to 4 embryos transferred and primary outcome evaluated was the newborn weight. We compared demographics and laboratorial-clinical outcomes to evaluate similarity between groups, and multiple logistic regression model was built to evaluate the association of Frozen-ET in the newborn weight adjusted for possible intervenient variables.
RESULTS: Groups were similar regards to body mass index (BMI) (Fresh-ET: 23.6±3.4Kg/m2 versus Frozen-ET: 23.4±3.6Kg/m2; p=0.605), multiple pregnancy (Fresh-ET: 29.5% versus Frozen-ET: 27.3%; p=0.457) and gestational age (Fresh-ET: 36.9±2.4 versus Frozen-ET: 37.2±2.6 weeks; p=0.158), except for women age (Fresh-ET: 34.8±5.1 versus Frozen-ET: 36.1±3.7; p<0.001).
Patients who received Frozen-ET presented a statistically higher newborn weight (Fresh-ET: 2.7±0.6 Kg versus Frozen-ET: 2.8±0.7 Kg; p=0.001).
Multiple linear regression confirmed that Frozen-ET is related to a higher newborn weight (Coef:0.104; p=0.001) adjusted for patients age (Coef:-0.002; p=0.438), BMI (Coef:0.004; p=0.305), multiple pregnancy (Coef: -0.391; p<0.001) and gestational age (Coef: 0.161; p<0.001).
CONCLUSIONS: Newborns from frozen-ET were 0.15kg heavier if compared to fresh-ET. Although significant, the mentioned difference did not affect, in both groups, the status of Appropriate for Gestational Age.
In spite our findings suggest that frozen cycles produce a better implantation environment when compared to fresh cycles, this approach does not represent a higher risk to produce Large for Gestational Age and its consequences. We may suggest that frozen-thawed embryo transfer is a safer method and do not influence the newborn weight status.
P-48. Nomogram of Antral Follicles X Score Age
R. S. A. Sasaki1, I. A. da Silveira1, M. C. S. Maia1, E. A. B. Fleury1, M. S. Approbato1
1Reproduction Human Laboratory. Federal University of Goias State, Brazil
OBJECTIVE: to construct a nomogram correlating age with absolute values of counts of antral follicles (CFA) of both ovaries of infertile anovulatory women.
MATERIALS AND METHODS: a cross-sectional retrospective study. We evaluated 86 patients who did not ovulate during the diagnostic exam of monitoring of ovulation, carried out between January 2013 and December 2014.
We excluded patients aged below 18 and above 38, women with FSH more than 10 IU/L, presence of follicles over 10mm in diameter on the first ultrasound monitoring, presence of endometriosis stages III and IV, hypo- and hyperthyroidism, prolactinaemia above 20 ng/ml, multipolicísticos ovaries (equal to or above 12 follicles), patients unilaterally ovariectomized or undergoing ovarian cystectomy, and smokers.
Data were tabulated using SPSS 23 and a linear regression was carried out to evaluate the effect of age on the antral follicle count. The level of significance was 5% (p <0.05).
RESULTS: The mean age was 33.12 years. The sum of antral follicles on both ovaries ranged 6-24, with an average of 13.60 per patient. The mean FSH dosage was 6.72 IU/L. The nomogram built showed a linear correlation between the age and the sum of both antral follicles of the ovaries.
CONCLUSIONS: A nomogram was constructed correlating linearly the reduction in the sum of both antral follicles of the ovaries with age in anovulatory patients.
Because patients with low ovarian reserve by FSH determination screened were excluded, and we don’t use percentiles, but absolute values of counts of antral follicles, this nomogram can be a simple reference for clinical and for future studies.
P-49. Quality Control in an IVF Laboratory
M. L. P. C. Silva1, B. O. Martins1, A. M. M. Cota1, M. Salvador1, R. M. Lamaita1,2
1Reprodução Humana -Mater Dei _ Belo Horizonte – Brasil
2Universidade Federal de Minas Gerais -UFMG - Belo Horizonte – Brasil
OBJECTIVE: To establish a literature review of the main points of QC in IVF laboratory. Quality control (QC) activities are designed to ensure that a specific element within the laboratory is correct. The main role of QC is to allow the repeatability and accuracy of results, providing an auditable system to ensure best practice in the laboratory. It is essential for the proper functioning of the laboratory, allowing for greater organization and security and is extremely important in an IVF laboratory.
REVIEW: The laboratory should have proper lighting; It is located in separate area with restricted access and the barrier locker room, being planned and constructed to facilitate cleaning, in addition to adequate size the number of procedures. The manipulation of gametes and embryos must take place in clean area, classified at least with ISO 5. Air quality is extremely important factor, so the need for filters and particle control. All procedures and standards should be clearly detailed in the manual, which must be constantly reviewed and updated. Temperatures laboratory incubators and must always be in normal ranges, should be avoided fluctuations. Moreover, it should take particular care to maintain the pH of the culture media because small changes in CO2 levels may have an effect on pH which influences embryonic development. There should be a routine daily internal QC, with verification of lots, expiration date; check and verify the identification of patients; registration of temperature and humidity laboratory; CO2 levels in incubators; temperature plates and hatcheries; cleaning of workplaces and dispose of waste properly. Every week, it should be slapping stock and liquid nitrogen level in the storage tanks.
CONCLUSIONS: The organization and structure of the IVF laboratory are essential steps to doing a good job in an assisted reproduction clinic. To ensure good good embryonic development and pregnancy rates to implement a good CQ is essential. It is vitally important as it provides as well as good results, safety for patients, clinical staff and laboratory staff.
P-50. Preimplantation Genetic Screening (PGS) by Blastocysts Biopsy for Embryo Selection in Brazil: Preliminary Results
M. Riboldi1, B. Coprerski1, M. Uehara1, C. L. Bandeira1, C. Simon2,3,4, C. Rubio2
1IGENOMIX Brasil Laboratório de Medicina Genética Ltda. São Paulo, Brasil
2IGENOMIX Valencia, Spain
3Universidad de Valencia, Valencia, Spain
4STANFORD, California, USA
OBJECTIVE: To evaluate the clinical outcome of preimplantation genetic screening (PGS) using array comparative genomic hybridization (aCGH) at different maternal ages in a Brazilian population.
MATERIALS AND METHODS: Infertility patients undergoing PGS cycles. All embryos were cultured to blastocyst stage and trophectoderm biopsy with aCGH analysis was performed. Trophectoderm samples from each embryo underwent whole genome amplification using the Sureplex Kit (BlueGnome,UK). Three groups were established according to the maternal age: A)25-35years (n=47); B)36-40years (n=91) and C)≥41years old (n=32). Statistical analysis was performed by qui-square.
RESULTS: We analyzed 170 cycles with 555 embryos with mean maternal age of 37.45±3.86, with the following results: The global rate of the abnormal embryos was 49.55% (n=275) and the incidence in the 3 groups was: A)41.28% (n=71), B)52.23% (n=152) and C)64.20% (n=52) (p=0.002). For single aneuploidy the result was 63.71% (n=172); and for the 3 groups we found the following results: A)71.43% (n=50), B)65.33% (n=98) and C)47.06% (n=24) (p=0.018). For double aneuploidy the result was 22.51% (n=61) and results for each group were: A)17.14% (n=12), B)24.00% (n=36) and C)25.49% (n=13) (p=0.448). For multiple aneuploidy the result was 14.02% (n=38); in the 3 groups the results were: A)11.43% (n=8), B)10.67% (n=16) and C)27.45% (n=14) (p=0.009). For chaotic embryos the results were 3.06% (n=17) and in the 3 groups were: A)2.91% (n=5), B)3.09% (n=9) and C)3.70% (n=3) (p=0.943). Mean number of embryos transferred was 1.47±0.57, with a pregnancy rate of 51.76% and implantation rate of 44.90%. The mean pregnancy and implantation rate, respectively, for the 3 groups were: A)53.19% and 42.55%; B)48.35% and 41.03 and C)59.38% and 59.38% (p=0.167 and p=0.547).
CONCLUSIONS: Increased incidence of aneuploidy blastocysts was observed with increasing maternal age, mostly due to an increased in the number of embryos with multiple aneuploidies. Nevertheless, similar pregnancy and implantation rates were achieved independently of the women age.
P-51. Donor Oocyte Characteristics Do Not Affect the Outcomes of a Oocytes Bank Program
A. P. Aquino1, T. S. Domingues1,2, T. G. Devechi1, C. Mata1, T. C. S. Bonetti1,2, E. L. A. Motta1,2
1Huntington Medicina Reprodutiva, Brasil
2Disciplina de Endocrinologia Ginecologica - Departamento de Ginecologia. Escola Paulista de Medicina - Universidade Federal de Sao Paulo, Brasil
OBJECTIVE: The increasing number of advanced age women looking for in vitro fertilization (IVF) treatment using donated oocytes prompt the need of oocyte donor bank. Among the advantages of oocyte donor programs are friendly cycles management and better donor selection, which stimulate it growing practice nowadays. The aim of this study was to evaluate the donor oocytes women characteristics and it influence in the recipients clinical outcomes in an oocyte banking program.
MATERIALS AND METHODS: This observational retrospective cohort study included 364 oocyte donation cycles carried out in 2013-2015 at private clinic in Brazil using an oocyte bank. All oocytes were vitrified and warmed using Kitazato protocols following manufacturer directions. Recipients underwent endometrium preparation with estradiol plus micronized progesterone according with standard protocols. Warmed oocytes were fertilized by intracytoplasmic sperm injection (ICSI), cultured until blastocyst phase and transferred on days 5 or 6 of embryo development. The multiple linear regression analysis evaluated the influence of donor characteristics in the clinical results of recipients.
RESULTS: Recipients were 42.0±4.8 years of age and the mean number of oocytes warmed was 8.9±2.3 per cycle. Oocyte survival and fertilization rates were 90.0% and 76.8% respectively. A mean of 54.9% of fertilized oocytes developed to blastocyst and 2.1±0.5 blastocysts were transferred per patient. Implantation rate was 28.2% and pregnancy was 55.9%. The oocyte donors presented the following characteristics: age (24.4±3.9), body mass index - BMI (24.3±4.2), antral follicle count (20.8±8.8), number of MII collected (24.6±14.9), previous pregnancy (55.3%) and ethnicity (83.7% of Caucasian). Any of donor characteristic were not associated to the pregnancy rate of recipients in a multiple logistic regression model (p>0.05), adjusted for recipients age, BMI, oocyte survival and blastocyst rates.
CONCLUSIONS: The patients screening for donor oocytes bank may be a strict process, mainly regards to age and BMI, in order to increase the chances of recipients pregnancy. This way, all patients in our oocyte bank program are young, with normal BMI, good ovarian reserve and consequently a satisfactory ovarian response after stimulation, resulting in a highly homogenous group with good prognosis, providing the establishment and development of an efficient donor egg bank.
P-52. Evaluation of the Efficiency of a Rapid Protocol of Seminal Cryopreservation
E. S. A. Velazquez1, C. R. Vaz1, E. S. De Araújo1, R. A. Salvador1, D. Til1 , V. L. L. Amaral1
1Universidade do Vale do Itajaí-SC (UNIVALI) - Brasil
OBJECTIVE: Evaluate the efficiency of a rapid protocol of seminal cryopreservation.
MATERIALS AND METHODS: This experimental study of validation of laboratorial technique has utilized 10 normozoospermic seminal samples. The samples have been divided in two aliquots of 0.4 mL and loaded in duplicates in straws of 0.5 mL. The volumes were diluted in Test Yolk Buffer (TYB, Irvine Scientific - IRVINE®) in proportion 1:1, the control group has been subjected to a conventional protocol of slow-cooling curve: 4ºC for 20 minutes, followed by 10 minutes in vapor of liquid nitrogen and thawing in 37ºC for 20 minutes. The other seminal aliquot from the test group has been subjected directly to cooling in vapor of liquid nitrogen for 10 minutes. Straws have been thawed by immersion on bain-marie, 72ºC for 7 seconds, followed by 37ºC for 30 seconds. After thawing of both groups the samples have been washed by centrifugation (600G) for 6 minutes in GV-hepes medium (Ingamed®). The supernatant was removed and the pellet resuspended in 0.3 mL in the same medium. There have been performed the final analyses of motility and vitality of the samples from both test and control groups. The recovery rates were statistically analyzed by t-Student test.
RESULTS: The average rates of motility and vitality recovery for test group were 66.2 % and 59.1%, respectively. These rates have not presented difference when compared to the rates of motility and vitality recovery from control group, which resulted in 60.6% and 60.9%, respectively.
CONCLUSIONS: The tested protocol in this study presented the same efficiency of sperm viability recovery as the conventional slow protocol and yet it has the advantage of decreasing the time expended for the performance of seminal cryopreservation.
P-53. Viability of Cryopreserved Seminal Samples Subjected to Brief Exposure to Room Temperature During Storing in Nitrogen
C. R. Vaz1, E. S. A. Velazquez1, E. S. De Araújo1, R. A. Salvador1, V. L. L. Amaral1, D. Til1
1Universidade do Vale do Itajaí-SC (UNIVALI) - Brasil
OBJECTIVE: Evaluate the viability of cryopreserved seminal samples, stored in liquid nitrogen, after brief exposure to room temperature, simulating the storing or withdrawal of other samples from the same rack.
MATERIALS AND METHODS: There have been utilized 9 normozoospermic seminal samples. The samples have been previously analyzed and forthwith cryopreserved in the diluting medium Test Yolk Buffer (TYB, Irvine Scientific - IRVINE®) in proportion 1:1 and packaged in straws of 0.5 mL, exposed to 4°C for 20 minutes, followed by 10 minutes in vapor of liquid nitrogen. The samples have been divided in 3 groups composed by 2 straws each one, and stored in the same rack. After the storing, the rack has been suspended and exposed to room temperature, for withdrawal of the straws from group 1, and hereupon the samples were returned to the nitrogen. After 30 minutes the rack has been suspended again for withdrawal of the straws from group 2, returning to the nitrogen once again. The same process has been performed for withdrawal of the straws from group 3. The time in which the rack has been remained suspended, was standardized in 10 seconds for all withdrawals. Straws have been thawed by maintaining all the samples at 37°C for 20 minutes, unloaded in GV-hepes (Ingamed®), centrifuged for 6 minutes at 600G and resuspended in 300 μL of the same medium. There have been evaluated the parameters of motility and vitality of the samples. The recovery rates have been compared by analysis of variance (ANOVA) and by Tukey’s test (significance level of 5%).
RESULTS: The average rates of motility recovery for groups 1, 2 and 3, were 64.6%; 46.2% and 51.8% respectively, while they were 59.1%; 51.3% and 57.1% for vitality, without substantial differences between groups.
CONCLUSIONS: The results of this study have demonstrated that little exposure, for brief period of time to room temperature, after seminal cryopreservation, has not altered motility or vitality of the samples after thawing.
P-54. Blastulation rate of MI oocytes matured and injected in D+1
V. M. Lopes1,2, N. I. Z. Tierno1,2, J. R. C. Lopes1,2, M. F. Roller1,2, A. C. F. F. Carneiro1,2, J. P. B. Brasileiro1,2
1Instituto Verhum, Brasilia, DF
2Cenafert, Salvador, BA
OBJECTIVE: Evaluate the results after ICSI using MI oocytes that reached MII stage that were injected in the day after the oocyte pick-up.
MATERIALS AND METHODS: A retrospective cohort study (January 2014-April 2015) of women ≤ 35 years, undergoing ICSI. Exclusion criterion: severe male factor (<1x106/ml) and patients with poor response (<5 MII oocytes). The MI oocytes were incubated with G1 plus or global culture media until the following day when the mature oocytes were injected. The resulting embryos were cultured until the sixth day after the oocyte pick-up. The results were analyzed by Excel.
Results: Of 63 eligible pacients, the average MI oocytes obtained by oocyte pick-up was 3.1 (197/63). Among the obtained 197 MI, 146 (74.1%) reached the stage MII in the next day, 58.9% (86/146) fertilized, 58.2% cleaved (85/146) and 16.4% (24/146) become blastocysts. The blastulation rate, defined by the ratio between numbers of blastocysts and number of mature oocytes cleaved, was 28.2% (24/85).
CONCLUSIONS: Even when using a non-specific embryo culture media for in vitro oocyte maturation the strategy to inseminate D + 1 can result in better use of oocytes in ICSI cycles. Therefore, it worth to rethink the habit of discarding the oocytes in MI stage after the oocyte pick-up.
P-55. The Impact of Age on Gestation, Implantation Rates and on Blastocyst Scoring, After Single and Double Embryo Transfers.
A. Bos-Mikich1, M. S. Michels1, C. G. Dutra2, N. P. de Oliveira2, D. Aquino1, N. Frantz2
1Department of Morphological Sciences, ICBS, Federal University of Rio Grande do Sul, Porto Alegre, RS, Brazil.
2Nilo Frantz Human Fertility Center, Porto Alegre, RS, Brazil
OBJECTIVE: The first aim of the present study was to assess the putative relationship between the age of the patient and blastocyst scores, in single (SET) or double (DET) transfer cycles. Second, we analyzed the effect of maternal age on clinical gestation and implantation rates after single and double blastocyst transfers.
MATERIALS AND METHODS: Retrospective analysis of fresh and cryopreserved cycles of assisted reproduction, in which patients received one or two blastocysts, between 2012 and 2014. Only cycles in which blastocyst grading scores were clearly registered were included. Clinical gestation and implantation rates were analyzed for SET and DET, where patients were divided into four age groups (<35, 35-37, 38-39, 40-42 years old). To analyze the impact of ICM, TE and EH scores on clinical gestation rates from SET or DET cycles that resulted in single (SETs) or twin (DETs) pregnancies, or non-gestations, patients were divided in two groups: < 35 and ≥35 years of age.
RESULTS: Our data demonstrate that for both, young (<35 years of age) and aged (≥35 years of age) women, TE score is the most important parameter to be assessed for embryo selection. However, inner cell mass (ICM) also plays an important role in blastocyst selection in the older group of patients. In addition, our data show that for young women the transfer of a single blastocyst results in similar gestational rates as DETs.
CONCLUSIONS: We suggest that blastocyst grading for patients aged 35 years or above shall be performed using a strict grading policy, possibly not of a single parameter, but TE, ICM and expansion grades together, to choose the “best combined-score blastocyst”. DETs should be considered in this group of age, particularly after previous cycles with pregnancy failures.
P-56. Are BMP15 Polymorphisms Risk Factors to Premature Ovarian Insufficiency?
M. Santos¹, S. O. Chiaratto¹, E. B. Cordts¹, C. P. Barbosa¹, D. M. Christofolini¹
1Instituto Ideia Fértil de Saúde Reprodutiva / Faculdade de Medicina do ABC – Santo André - Brasil
OBJECTIVE: To compare the incidence of the BMP15 gene polymorphisms in patients with POI, patients with elevated levels of FSH and controls and contribute to the elucidation of the etiology of POI.
MATERIALS AND METHODS: We analyzed 100 women with FSH> 25 mUi/mL (case group 1), 65 women with FSH levels between 10 and 25 mUi/mL (case group 2) and 100 fertile women with no personal or family history of premature menopause (controls). Genotyping for polymorphisms rs3897937, rs3810682 and rs17003221 the BMP15 gene was performed by qPCR from DNA extracted from peripheral blood. The results were statistically analyzed using the chisquare test BioEstat 5.3 software.
RESULTS: For the polymorphism rs3897937 observe the following distribution of genotypes GG/GA/AA in the case group 1: 17, 33, 31; in the case group 2: 7, 25, 20 and in the control group: 14, 38, 39. There was no significant difference in the incidence of genotypes between groups 1 (p = 0.613) and 2 (p = 0.764) and controls. For the polymorphism rs3810682 observe the following distribution of genotypes CC/CG/CG: 57, 29 and 0 in the case group 1; 35, 16 and 1 for group 2, and 71, 24 and 0 in the controls. There was no significant difference in the incidence of genotypes between groups 1 (p = 0.212) and 2 (p = 0.292) and controls. For the polymorphism rs17003221 observe the following distribution of genotypes TT/TC/CC in the case group 1: 7, 60, 23; in the case group 2: 0, 33, 21; and in the control group: 18, 39, 23. For this polymorphism showed significant differences between groups 1 (p = 0.0127) and 2 (p = 0.0009) and controls.
CONCLUSIONS: There are only four studies in the literature investigating the contribution of BMP15 gene in POI and the findings are contradictory. In the present study reinforce the role of the gene as a possible risk marker for ovarian dysfunction.
P-57. Comparative Evaluation of survival rates thawing and Pregnancy coming from women embryos SHO, elevated Serum Progesterone on the day of HCG or with surplus Embryos. In thawed Embryo transfer cycles: Retrospective Study
M. Santos1, V. M. B. C. Lins1, C. Z. Berton1, W. Carvalho1, C. P. Barbosa1
1Instituto Ideia Fértil de Saúde Reprodutiva – Faculdade de Medicina do ABC – Santo André - Brasil
OBJECTIVE: To evaluate survival rate after thawing embryos undergoing vitrification due to ovarian hyperstimulation syndrome (OHSS), elevated serum progesterone on the day of HCG and excess embryos. Evaluate the pregnancy rate between the groups.
MATERIALS AND METHODS: A retrospective study of 281 women undergoing treatment for Assisted Reproduction (ART), the same were divided into three groups, according to the indication of freezing, groups were: OHSS (129 patients), serum progesterone high (57 patients) and excess embryos (95 patients). Of these patients, 488 embryos were studied, 246 (OHSS), 107 (high progesterone) and 135 (excess embryos). Inclusion criteria were age ≤ 40 years, serum FSH ≤ 10 mUI/ml and the presence of one or more vitrified embryos. Were excluded patients with endometriosis III/IV, with genetic alterations and severe male factors.
All embryos are coming from normal fertilization (two pronuclei on day 1) by intracytoplasmic sperm injection technique.All embryos were vitrified and thawed by the same team of embryologists using Irvine Kit and respecting the manufacturer’s recommendations. All embryo transfers were performed by the same team gynecologists and with the same type of catheter. Statistical analysis was performed using SPSS for Windows 11.0, considered as significant p <0.05.
RESULTS: The results revealed statistically lower survival rate in vitrified embryos by high progesterone group (mean 86.1; CI 81.2- 91.0) versus OHSS (91.9, CI 89.2-94.5) versus excess (92.9, CI 88.7-97.1), p <0.01. And statistically higher pregnancy rate in vitrified by high progesterone group (86%) versus 65% (OHSS) versus 66% (excess), p = 0.01.
CONCLUSIONS: The vitrified embryos coming from women with high progesterone serum levels had lower survival rate, but higher pregnancy rate compared to other groups.
P-58. In vitro culture of fresh bovine preantral follicles in alginate three-dimensional matrix (3D)
J. S. Guedes1,2, J. K. Rodrigues1, A. L. M. Campos1,2, J. P. J. Caetano1,2, R. M. Marinho1,2
1Pró-Criar Medicina Reprodutiva – Belo Horizonte - Brasil
2Pós-graduação - Faculdade de Ciências Médicas de Minas Gerais - Brasil
OBJECTIVE: Evaluation of survival, growth and antrum formation of bovine preantral follicles (secondary and multilayer) during in vitro 3D matrix culture.
MATERIALS AND METHODS: There were isolated 51 follicles from bovine ovaries (N = 4): 11 were secondary, with a diameter between 125 and 250 μm and 11 multilayer with diameter between 250 and 400 μm.
The follicles were treated with collagenase enzyme (1mg/ml) and then mechanically dissected using scissors, tissue slicer and 23G/26G needles.
Only follicles with an intact basal membrane, a visible rounded oocyte centrally located inside the follicle and which had no antral cavity were selected.
The follicles were individually encapsulated in alginate matrix, maintained in culture medium supplemented with FSH (150ng/ml), insulin (1mg/ml), transferrin (1mg/ml), sodium selenite (50ug/ml), synthetic serum substitute (0.3%) and antibiotic gentamycin (10mg/ml), and their development was followed over 20 days.
RESULTS: The follicle survival was 43%. From the total of 51 follicles, 22 survived until the 20th day of culture.
The follicles had initial average diameter of 265.9 ± 93.8 μm and 413 μm ± 100.2 at the end of culture, presenting an increase of 1,5 times the initial size.
The antrum formation rate was 86%, usually starting around the 7th day of culture.
CONCLUSIONS: The preliminary results demonstrate the potential of the in vitro development of fresh bovine secondary follicles to the antral stage. The bovine has shown a great translational model for the development of ovarian cryopreservation techniques and follicle maturation in humans. A larger sample will give more information to use the technique in human ovarian tissue.
P-59. Regular Menstrual Cycles in Anovulatory Patients
R. S. A. Sasaki1, I. A. da Silveira1, M. C. S. Maia1, E. A. de Barros Fleury e Ferreira Fleury1, M. S. Approbato1
1Reproduction Human Laboratory. Federal University of Goias State, Brazil
OBJECTIVE: To evaluate whether anovulatory patients during the diagnostic exam of monitoring of ovulation reported having regular or irregular cycles previously.
MATERIALS AND METHODS: A retrospective study of prevalence. We evaluated 86 patients who did not ovulate during the diagnostic exam of monitoring of ovulation, carried out between January 2013 and December 2014. It was later sought the information in the records if these patients reported having regular cycles or non-scheduled (irregular or amenorrhea).
We excluded patients aged below 18 and above 38, women with FSH more than 10 IU/L, presence of follicles over 10mm in diameter on the first ultrasound monitoring, presence of endometriosis stages III and IV, hypo- and hyperthyroidism, prolactinaemia above 20 ng/ml, multipolicísticos ovaries (equal to or above 12 follicles), patients unilaterally ovariectomized or undergoing ovarian cystectomy, and smokers.
Data were tabulated using SPSS 23 and calculated the prevalence of anovulatory patients who reported having regular cycles and who reported having irregular menstrual cycle or amenorrhea.
RESULTS: 86 patients were raised that did not ovulate during the examination of monitoring ovulation, and of these, 66 reported having regular cycles (76.74%) and 20 reported irregular cycles or amenorrhea (23.26%).
CONCLUSIONS: The reporting of regular menstrual cycles between anovulatory patients was frequent, and few reported irregular cycles.
P-60. Mild Elevated Prolactin Effect of Ovulation in Infertile Women with Regular Menstrual Cycles, According Progesterone Levels
E. G. M. Sanchez1, C. R. Giviziez1, H. M. Sanchez1, M. C. S. Maia1, I. A. da Silveira1, M. S. Approbato1
1UFG -Universidade Federal de Goiás -Brasil
OBJECTIVE: Evaluate the influence of moderate levels of prolactin (21-29 ng/ml) in ovulation of infertile womens with regular cycles evaluated by progesterone levels.
MATERIALS AND METHODS: Study of case-control. The sample consisted of 343 womens with ages ranging from 20 to 40 years who were treated from 2000 to 2014 in laboratory of human reproduction and private clinic of Gynecology and Obstetrics of in Goiás. Where the exposure factor was the moderate elevation of prolactin and the outcome was anovulation. Analyses were made of the physical records stored Medical and electronics. The participants were women who had dosage of PRL and P4. The patients were classified according to the status estimated by the ovulatory dose of progesterone (P4 ≥18nmol / l and ≥ 5.65 ng / ml) and were divided into two groups: (1) a likely ovulation and (2) likely to anovulation. In groups 1 (n=284) and 2 (n=59) were compared with the percentages of patients who do not ovulate with normal prolactin (3 to 20 ng / ml) versus moderately elevated prolactin (21 to 29 ng / ml). It was performed comparability age, body mass index, height, weight, infertility duration, FSH (ng / ml) TSH (mIU / l) LH (IU / l) and Estradiol (ng / dl) between the groups. Statistical analysis was performed using IBM SPSS Statistics 20.0 software and Bioestat (version 5.3). To assess differences between proportions used the chi square test. Was the level of significance p <0.05.
RESULTS: The results demonstrated that moderate elevation of prolactin (21-29 ng / ml) caused a significant reduction (p = 0.03) in the ovulation rate of infertile patients with regular cycles based criterion as ovulation progesterone levels ≥ 5,65 ng / ml.
CONCLUSIONS: Prolactin has important effect on the regulation of reproduction and its moderate increase may negatively affect ovulation infertile women with regular cycles.
P-61. A Retrospective Cohort Study of Pregnancy Outcome in women with Recurrent Pregnancy losses with at least five Miscarriages
N. M. Attia1, D. R. Ritsick1, C. Bommer1, J. Braverman1
1Braverman Reproductive Immunology PC - New York - USA
OBJECTIVE: There has been much debate in the obstetrical field on when it is necessary to treat recurrent pregnancy loss and if treatments improve outcome. To this end we have learned that aneuploid miscarriages are not predictive of further miscarriages while euploid miscarriages are predictive of further miscarriages, suggesting that the euploid group requires treatment.
The literature shows that women with 5 or more miscarriages are most likely having euploid losses. The objective of the study was to assess retrospectively the pregnancy outcome of women under our care with a history of at least 5 miscarriages.
MATERIALS AND METHODS: A total of 30 women with 5 or more miscarriages were included in the study. The only exclusions were uterine anomalies. Full HLA typing as well as an extensive immunologic panel were performed on each patient. History of documented euploid losses for each patient was recorded as well.
Patients received our tailored immune therapy based on these results prior to conception (natural conception or IVF cycle), and the treatment was maintained at least through the first trimester Pregnancy outcome was recorded retrospectively with a pregnancy success being defined as a live birth or an ongoing pregnancy of more than 20 weeks. Fisher exact test with a two-tailed probability was used to analyze the results. P< .05 was considered statistically different.
RESULTS: The mean age of our patients was 33.5 years old. Prior to our care, 90% of the patients had at least one documented euploid loss (p=.00001) among all their losses. With our immune therapies, 80 % have had at least one successful pregnancy (p=.0003) with a maximum of three attempts and 60% were successful at the first attempt (p=.22). Among the losses, 82% were documented and all were aneuploid.
CONCLUSIONS: Besides our outstanding pregnancy success rate at first attempt (60%) and even greater rate (80%) after adjusting our therapy regimen, it is important to underline that none of the documented losses were euploid showing that our immune therapies are highly effective in retaining euploid pregnancies.
P-62. Nursing Diagnoses of patients at risk of develop-
ing Ovarian Hyperstimulation Syndrome of: Case Report
T. O. Figueiredo1, J. Assi1, C. Mata1, M. Ferrari1
1Huntington Centro de Medicina Reprodutiva – São Paulo – Brasil
INTRODUCTION: The failure to conceive affects approximately 15-20% of reproductive aged couples. In Vitro Fertilization (IVF) is one of the techniques used in assisted reproduction to improve the chances of achieving pregnancy. The cycle is carried out with ovarian stimulation for growth of multiple follicles and are obtained during surgery. The ovarian hyperstimulation syndrome (OHSS) is an important complication of assisted reproduction techniques due to their high morbidity. The pathogenesis is linked to the action of vasoactive substances that are secreted under gonadotrophin stimulation and generate increased vascular permeability with intravascular volume depletion and massive leakage of protein rich fluid into the peritoneal space, the pleural space and, more rarely, the pericardial space.
CASE REPORT: In view of this, it is necessary to effective nursing work, with the intention of identifying risks to the development of OHSS in preventive. Therefore, it is necessary to develop all stages of Nursing Care Systematization (NCS) in its entirety, so were identified possible diagnoses nursing classified under North American Nursing Diagnosis Association - NANDA in patients at risk of developing OHSS order to analyze whether the diagnoses existing is sufficient to classify the syndrome risk factors, creating the possibilities of nurses in elaborate more effective preventive action. Only five diagnoses were selected.
COMMENTS: specific risk factors for OHSS are not included in NANDA the related factors, which would enable the early identification of patients in this group. NANDA presents diagnostics for the care of the patient who has developed the syndrome, leaving the desired prevention. There is the need to create new specific diagnostic area for human reproduction.
P-63. The Chemokine Receptor-2 (CCR2) deficiency leads in Reduced Follicular Activation and Fertility
A. G. A. Santos1, C. P. Almeida2, R. C. Russo2, J. H. M. Viana3, P. H. A. Campos-Junior1
1Laboratório de Morfofisiologia Gonadal e Reprodução Assistida - Universidade Federal de São João Del Rei – São João Del Rei – Minas Gerais
2Laboratório de Imunologia Pulmonar – Universidade Federal de Minas Gerais – Belo Horizonte - Minas Gerais
3Laboratório de Reprodução Animal – Embrapa Gado de Leite – Juiz de Fora – Minas Gerais
OBJECTIVE: In recent studies performed by our group, we observed the expression of CCR2 in the mice and human testes, and that the CCR2 deficiency causes a drastic reduction in daily sperm production. However, it is not identified the role of this chemokine-receptor interaction in ovarian homeostasis. In this scenario, the aim of this study was to investigate the CCR2 expression in wild-type mice ovaries (WT), quantify the ovarian follicular population, recruitment rates and follicular atresia in WT and CCR2-/- mice.
MATERIALS AND METHODS: Ovaries were collected from female (60 days-old) WT (n=10) and CCR2-/- (n=10) mice and processed for morphometric analysis, follicular quantification, immunohistochemistry, and western blotting. The mean number of litters per breeding female and the number of pups per litter (during 1 year) also were evaluated. All data were compared using the t test.
RESULTS: The CCR2 protein was observed in the WT ovarian lysate and was not observed in CCR2-/-; while the β-actin expression (control) was observed in both groups. Using immunohistochemistry analyses the CCR2 expression was not observed in primordial follicles. However, this receptor was immunolocalized in oocytes included in growing follicles: primary, secondary, antral and atretic. Although body and ovarian weight and gonadal-somatic index were not different between the groups (P>0.05), the CCR2 deficiency leads in ovarian follicular population modifications. The CCR2-/- showed ovarian follicular reserve ~40% higher than WT (P<0.01). However, there was a reduction (~50%) in the number of preantral follicles (P<0.01), while the number of antral follicles was not different (P>0.05). Corroborating these findings, lower activation and follicular atresia index and fewer litters/breeding female were observed in CCR2-/- (P<0.01).
CONCLUSIONS: Overall, this study demonstrates for the first time in the literature, that (i) the CCR2 is a phenotypic marker and a potential regulator of follicular activation, (ii) CCR2 regulates mainly the early stages of folliculogenesis, and (iii) CCR2 deficiency can leads to a significant reduction in fertility. Finally, this study indicates that the effects of CCR2 antagonists in folliculogenesis should be carefully studied before their commercialization. CEUA 27/2014.
P-64. Hysteroscopic Findings in Asymptomatic Infertility Patients
S. A. de Oliveira1, G. M. Coelho1, M. S. Borges1, I. A. Rocha1
1Instituto Valenciano de Infertilidade - IVI Salvador - Brasil
OBJECTIVE: to assess the prevalence of uterine changes in hysteroscopic examinations of asymptomatic patients diagnosed with infertility. Uterine diseases can cause infertility as well as reduce pregnancy rates in assisted reproduction. Some observational studies suggest that there is an increased pregnancy rate after hysteroscopic resection of endometrial polyps, submucosal fibroids, uterine septum or adhesions. However, the use of hysteroscopy in Human Reproduction is still widely discussed.
MATERIALS AND METHODS: we performed a prospective study from January 2014 to May 2015, being made diagnostic and surgical hysteroscopy in two groups of patients in the Instituto Valenciano de Infertilidade - Salvador. Group 1: asymptomatic patients with a history of previous uterine surgery (curettage, cesarean section, myomectomy, polypectomy) that would be subjected to ICSI cycle with own oocytes; group 2: patients with asymptomatic ICSI statement with donor oocytes.
All alterations were treated by surgical hysteroscopy and it was performed a percentage calculation of hysteroscopic findings.
RESULTS: Group 1 had a total of 98 patients, 41% of patients had a change in hysteroscopy, as follows: synechia (42%), endometrial polyps (18%), submucosal fibroids (10%), intrauterine septum (10%), uterine bending (10%), cervical stenosis (5%), mucocele (3%) and istmocele (2%). In group 2, there were a total of 21 patients, 38% of these patients had uterine pathologies, which were: endometrial polyps (38%), submucosal fibroids (25%), bowing (13%), adenomyosis (12%) and synechia (12%).
CONCLUSIONS: The results of this study show that uterine pathologies are found with high frequency in patients diagnosed with infertility, even asymptomatic, justifying performing hysteroscopy systematically. In addition, there was an increase in implantation rate after hysteroscopy in patients with implantation failure in a previous cycle, but it was not possible to say that such an outcome was related to hysteroscopy or a significant difference statistically. There are no randomized, controlled, prospective sufficient to prove that the treatment of these conditions improves the prognosis of the patient. However, observational studies have suggested benefit of resection of submucosal leiomyomas, adhesions and polyps, improving pregnancy rate.
P-65. Blastulation and AMH
E. De Conto1,2, D. S. da Silva1, V. K. Genro1, R. Chapon1,2, J. S. L. da Cunha Filho1,2
1INSEMINE Center of Human Reproduction, Porto Alegre, RS, Brazil
2Hospital de Clínicas de Porto Alegre - HCPA/ Universidade Federal do Rio Grande do Sul - UFRGS, Porto Alegre, RS, Brazil
OBJECTIVES: Determine the blastulation rate (BR) with respect to age, serum levels of anti-Müllerian hormone (AMH) and Follicle Stimulating Hormone (FSH) and number of oocytes retrieved in assisted reproduction techniques (ART).
MATERIALS AND METHODS: Prospective study selected a population of good responder patients including 59 cycles of ART January 2013 to May 2015. Statistical analysis: t test for independent samples and Levene test, p<0.05 statistically significant.
RESULTS: Considering two groups: BR0 with BR<0.5 and BR1 with BR≥0.5; the results (mean ± standard deviation) were, respectively, patient age: 34.5±5.0 and 34.9±3.5 years old, FSH concentration: 6.35±1.5UI and 7.35±3.1UI, AMH concentration: 5.97±4.8ng/mL and 3.54±2.4ng/mL and number of oocytes retrieved: 9.57± 3.6 and 7.58 ± 3.5.
CONCLUSIONS: We demonstrated that AMH concentration determines different blastulation rates in good responder groups with similar FSH serum levels. The group with the largest number of oocytes, predictable event for its AMH high concentration relative to the other, has less BR, this may be a result of the erratic recruitment of follicles in hormonal induction: as largest oocytes retrieved increases the chance to incompetent oocytes who can have nuclear or cytoplasmic maturation not complete, abnormal distribution of cytoplasmic organelles thus presenting failures in fertilization or blocking in embryonic development, not reaching the blastocyst stage, also cannot rule out the possibility of genetic damage. We therefore conclude that patients with AMH between 1.14-5.94ng/mL has a greater chance to form blastocyst than patients with higher concentrations of this hormone and which AMH could be used as predictor for the formation of blastocyst in the conduct of ART cycles in patients with good prognosis.
P-66. Comparison of Embryos Quality of One Laboratory of ISO 5 and 7 Class with Embryos of a Conventional IVF Laboratory, in Patients Submitted to ICSI
M. Approbato1, T. M. da Silva1, M. Ramos1, M. Canedo1, I. A. da Silveira1, F. C. Approbato1
1Reproduction Human Laboratory, Federal University of Goias State, Brazil
OBJECTIVE: Since 2006 with the publication of RDC 33 and in 2011 with the publication of RDC 23, the Brazilian Government Regulatory Agency ANVISA determined that in vitro laboratories should obey rigid criteria to manipulate human embryos and gametes. This paper compares the previous conventional IVF laboratory results with the new one with ISO 5 (Class 100) and ISO 7 (Class 10.000) certification.
MATERIALS AND METHODS: A Cross-sectional study, comparing 71 patients, a total of 102 embryos. Torn or VG oocytes were not included. (Group 1) 71 patients treated in conventional Laboratory (33 patients with TMSP – Total Mobile Sperm Processed <= 1,0 x 106, and 38 with TMPS >= 12 x106). Group 2: 31 patients treated in ISO 5 and ISO 7 certified laboratory (15 with TMSP – Total Mobile Sperm Processed <= 1,0 x 106, and 16 with TMPS >= 12 x106). Both groups were inseminated by ICSI technique. The following variables were included: embryo quality (percentage of A grade embryo or morula on D3 post ovum pick up, Depa-Martynow et al, 2007), and percentage of embryo formation. The following variables (confound factors) were paired: Age, BMI, Infertility duration (months), basal FSH, basal Estradiol and TMPS. It was used the Mann-Whitney U and Chi-Square test statistics (p = 0,05). Calculations were done with SPSS 17.0.
RESULTS: There was an average of embryo formation of 43,48 % (+/- 33,28 SD) in ISO 5/7 Class and 33,57 % (+/- 32,85 SD) in Standard Laboratory, statistically not significant. There was an average of Grade A or Morula of 32,30 % (34,99 SD) in ISO 5/7 Class and 26,74 % (29,69 SD) in Standard Laboratory, statistically not significant.
CONCLUSIONS: Though ISO 5/7 Class laboratory has improved the percentage of embryo formation and Grade A / Morula this elevation was not statistically significant. The high variability of the groups probably may be explained by the inclusion of a very low sperm count group, interfering with groups’ comparability. In future studies, we will consider separate groups with normal and low TMPS.
P-67. Case Report: Hormone Therapy for Spermatogenesis Induction in Patients with non-obstructive Azoospermia (NOA)
R. A. C. Monteiro1,2,3, J. R. Pariz1,2,3, J. A. Monte4; I. Ciccone5, J. Hallak1,2,3
1Laboratório Androscience, SP-SP
2Setor de Andrologia, Departamento de Urologia da FMUSP, SP-SP
3Unidade de Toxicologia Reprodutiva, Departamento de Patologia da FMUSP, SP-SP
4Setor de Enfermagem da Clínica JH, SP-SP
5Setor de Nutrição da Clínica JH, SP-SP
INTRODUCTION: Non-obstructive azoospermia (NOA) affects 10% of all men with infertility and is responsible for 80% in the subgroup of men with azoospermia, while obstructive azoospermia contributes to 20% of this subpopulation of infertile men. Treatment of patients with NOA needs correct diagnosis and induction of spermatogenesis to try to produce viable sperm ejaculation.
CASE REPORT: Patient 29 years, married for three years, planning pregnancy a year ago, forwarded diagnosed with NOA. Reported prior execution of aspiration of the right testicle, in which the report relates 20 seminiferous tubules with irregular shape and size, decreased germ cell, absence of sperm in the lumen of the tubules. In genetic analysis, karyotype 46XY, Y without microdeletions. Historical and physical examination of the patient was carried out and requested laboratory tests which included hormone levels and semen analysis, in which showed bilateral varicocele, hypogonadism, vitamin D deficiency and severe oligozoospermia with sperm isolated (observed a sperm every five drops of 5μl). It was adopted stimulation of spermatogenesis with recombinant FSH (r-hFSH), human chorionic gonadotropin (hCG), Vitamin D and nutritional supplementation. After the treatment, there was considerable progress with rare presence of sperm in fresh seminal sample evaluation (5 observed sperm / 5μl). Although a significant number of sperm in the sample, microsurgery (microTESE) was also considered, because the number of sperm was in very limited and low morphological quality. Continuity of treatment for over two months was considered by patient to avoid surgery. After time proposed were performed with three ICSI, with 2 cryopreserved embryos for later transfer.
COMMENTS: With the results of this case report we suggest that supplementation with hCG and r-hFSH, and nutritional intervention enhances spermatogenesis, as we observe a significant sperm count increase (5 times the initial concentration), demonstrating the effectiveness in the conduct proposal. Thus, the study shows that this protocol can be adopted in the management of patients diagnosed with severe oligozoospermia sent to Assisted Reproduction.
P-68. Finasteride 1mg/Daily Consumption Impairs Spermatogenesis by Histological Evaluation and Semen Quality in Men in Reproductive Age
J. R. Pariz1,2,3, R. A. C. Monteiro1,2,3, J. Hallak1,2,3
1Laboratório Androscience, SP - Brasil
2Setor de Andrologia, Departamento de Urologia da FMUSP, SP - Brasil
3Unidade de Toxicologia Reprodutiva, Departamento de Patologia da FMUSP, SP – Brasil
OBJECTIVE: To study the effect of finasteride 1mg/daily consumption on the spermatogenesis and seminal quality. Finasteride, an oral type 2,5 α-reductase inhibitor, is used in 1 mg/daily doses for the treatment of male pattern hair loss. Its consumption affects the conversion of testosterone to dihydrotestosterone (DHT), which is a more potent androgen, impairing the male reproductive system.
MATERIAL AND METHODS: We studied 23 male subjects (mean 33 y.o.) who came for an initial andrological evaluation and who self-reported use of finasteride 1mg for more than one year. These subjects were paired and compared, by Paired-Samples T Test (p adopted <0.05), with fertile (pre-vasectomy candidates with no risk factors for sperm/testicular dysfunction) and infertile (for over a year) patients with same age and varicocele grade. In addition, we included six testicular biopsies with spermatogenesis assessment.
The study was approved in Ethics Committee (n°12331). We conducted ANOVA test of the means and adopted
p <0.05.
RESULTS: The mean of Finasteride consumption was 72.22 mouths. Finasteride users had significantly decreased in total sperm count (p=0.026 and 0.014) and total motile sperm count (p=0.053 and 0.036) when compared with infertile and fertile group, respectively. Furthermore, morphology by strict (p=0.001) and WHO (p<0.001) criteria and testicular volume (p<0.001) decreases in Finasteride users when compared with fertile men. Creatine-kinase activity which is a marker of sperm immaturity was increased in Finasteride users (p<0.001). In spermatogenesis analysis, four showed spermatogenesis altered and round spermatids; predominant Johnsen score was 7. We conducted ANOVA test of the means adopted and p <0.05.
CONCLUSIONS: Our results demonstrate that Finasteride consumption affects negatively the spermatogenesis and semen quality and may be contraindicated to young men that are willing to father their own offspring. We do not yet know the long-term effects on male reproductive health and recovery rate after discontinuation, but this study suggest that Finasteride is of concern for the proportion and widespread prescription by dermatologists and others health professionals unaware of its potential reproductive effects.
P-69. Dissecting Sperm function in Primary ciliary Dyskinesia in Male Infertility: A Case Report
J. R. Pariz1,2,3, H. E. Chemes4, R. A. C. Monteiro1,2,3, J. Hallak1,2,3
1Laboratório Androscience, SP, Brazil
2Setor de Andrologia, Departamento de Urologia da FMUSP, SP, Brazil
3Unidade de Toxicologia Reprodutiva, Departamento de Patologia da FMUSP, SP, Brazil
4Centro de Investigaciones Endocrinológicas, CEDIE-CONICET, Buenos Aires, Argentina
INTRODUCTION: Primary ciliary dyskinesia (PCD) is a medical condition characterized by ciliary dysfunction and impaired mucociliary clearance resulting also in male infertility due to total absence of sperm motility.
CASE REPORT: A 26-year-old man, 66kg, 179cm, asthmatic, report primary ciliary dyskinesia with situs inversus and infertility. In the seminal analysis, showed normal macroscopic parameters, with pH 8.0 and 5.0 ml of seminal volume. The sperm concentration was 33 million/ml and total number of sperm was 165 million, however, was no observed motile sperm. In sperm morphology analysis, we observed only amorphous sperms, with most round tail. In complementary fertility investigation, were performed round cells count and qualitative fructose tests, not altered, and the sperm vitality evaluation by Hoechst-33258 fluorescent stain showed 88% of viable sperm. In addition, the quantification of reactive oxygen species (ROS) and malonaldehyde showed oxidative equilibrium and low lipid peroxidation of sperm membrane, with ROS=0.14x104com/20x104 spermatozoa and TBARS= 182.69mg x 105 of TBARS/106 spermatozoa. Creatine kinase enzyme activity was 0.05U/108spermatozoa, normal. Mitochondrial activity was evaluated by 3,3-diaminobenzidine, however, is not possible analyzed because the mid-piece of spermatozoa not stained. Finally, ultrastructural morphologic characteristics examination by electron microscopy demonstrated the existence of serious alterations of sperm flagella, with profile thick and very irregular. The normal 9+2 structure of the axoneme was distorted and most microtubule profiles were completely obliterated. When microtubules were present it was evident that central pairs were absent (9+0 configurations). Dynein arms could not be examined due to flagellar modifications. The fibrous sheath was hypertrophied with serious disruption of flagellar ultrastructure. Mitochondrial pieces were present. Alterations in chromatin maturation and compaction were present in 38% spermatozoa (nuclear rarefactions or “vacuoles”). Normal chromatin organization was seen in 52% spermatozoa.
COMMENTS: We report the first case in the literature to dissect sperm function in order to try to establish a predictive prognostic value to council these patients how to proceed in the reproductive arena. This study reinforces the hypothesis that PCD affects only the morphologic structure, compromising its motility and mitochondrial activity, whereas oxidative equilibrium and sperm viability showed
preserved.
P-70. Expression of PGR, HBEGF, ITGAV, ITGB3 and SPP1 Genes in Eutopic Endometrium of Infertile Women with Endometriosis
M. G. Da Broi1, C. V. Rocha Jr1, W. P. Martins1, J. Meola1, R. A. Ferriani1, P. A. Navarro1
1Setor de Reprodução Humana, Departamento de Ginecologia e Obstetrícia, Faculdade de Medicina de Ribeirão Preto (FMRP) – USP
OBJECTIVE: It is believed that the impairment of endometrial receptivity may be one of the mechanisms involved in the etiopathogenesis of endometriosis-related infertility. Studies have shown alterations in the expression of genes related to embryo implantation in women with the disease. Progesterone plays a key role in the molecular changes that promote endometrial receptivity; however, these patients seem to present a progestin resistance. We question alterations in the progesterone receptor gene (PGR) expression and consequently in the expression of genes directly or indirectly regulated by its ligand, including HBEGF (epidermal growth factor linked to heparin), ITGAV and ITGB3 (integrin αvβ3) and SPP1 (osteopontin), which are related to endometrium-embryo interaction. The objective of this study was to compare the expression of PGR, HBEGF, ITGAV, ITGB3 and SPP1 genes in eutopic endometrium of infertile women with endometriosis and fertile and infertile controls during the window of implantation.
MATERIALS AND METHODS: Endometrial biopsies were performed in 15 patients (5 infertile with endometriosis, 5 fertile controls and 5 infertile controls), between the 6th and the 12th day after ovulation, with histological dating performed by experienced pathologist, according to Noyes criteria. Total RNA extraction, cDNA synthesis and gene expression analysis by Real-Time PCR were performed. For comparisons, we used the Kruskal-Wallis test at 5% significance level.
RESULTS: There was no significant difference in the expression of any studied gene when comparing the endometriosis, fertile control and infertile control groups. The present sample size allows us to exclude, at least, a big difference in the expression of the evaluated genes in the groups.
CONCLUSIONS: Infertile patients with endometriosis seem to have no changes in PGR, HBEGF, ITGAV, ITGB3 and SPP1 expression when considering a big difference among the groups. Larger studies are needed to investigate the presence of moderate or small difference.
Support: FAPESP (2011 / 17614-6), Brazil, CNPq (471943 / 2012-6; 140137 / 2015-7), Brazil.
P-71. Spermatogenesis Induction Associated with Mechanical Crushing Technique and Testicular Biopsy Incubation Results in Pregnancy: A Case of Obstructive Azoospermia
R. A. C. Monteiro1, J. R. Pariz1,2,3, G. L. Souza1, J. Hallak1,2,3
1Laboratório Androscience, SP
2Setor de Andrologia, Departamento de Urologia da FMUSP, SP
3Unidade de Toxicologia Reprodutiva, Departamento de Patologia da FMUSP, SP
INTRODUCTION: Recent advances in the diagnosis and laboratory techniques applied induction of spermatogenesis in men with azoospermia or severe oligozoospermia has provided significant improvement in semen quality.
CASE REPORT: ACR, 46 years old, married for the third time, secondary infertility and current wife of 31 years. Presented correction bilateral varicocele, vasectomy and previous ICSI with epididymal punch without success.
After detailed history and semen analysis stablished, obstructive azoospermia, iatrogenia and bilateral varicocele was diagnosed. The patient underwent microsurgical exploration of the epididymis (MESA) and microTESE and found rare immotile sperm in MESA material and rare non-progressive sperm in microTESE.
The samples were processed and cryopreserved without mechanical grinding. After six months, MESA samples were thawed and observed only immotile sperm, sent to ICSI. Only one embryo was cryopreserved (1 blastomere with 2 nucleous). The case was discussed by the team and the couple and adopted spermatogenesis stimulation with hCG, supplementation with vitamin D and new microTESE.
Observed improvement in spermatogenesis with Jhonsen index of 1 to 5.
Testicular tissue fragments were analyzed in the surgical field, mechanical trituration processed and observed 1.3x106 sperm/ml and 10% non-progressive motility. Removal of cell debris were carried out lysis erythrocytes, enzyme digestion and 0.9x106 sperm/ml was observed with 20% motility.
Samples were supplemented with 1% human serum albumin (HSA) and after a period of 18 hours incubation in 5% CO2, all samples were cryopreserved.
After six months, samples were thawed to ICSI and observed non-progressive sperm that were injected into an embryo obtained and (T + 5), transferred to the patient, along with the first embryo cryopreserved, and the procedure success was demonstrated by gestation.
COMMENTS: The case shows that multidisciplinary treatment of male reproductive health has improved the quality of spermatogenesis, portrayed by Johnsen index. Associated with this, dedicated protocol to cases of azoospermia, with exhaustive search of sperm, enzymatic digestion and incubation enabled the identification of mobile sperm and increased the probability of pregnancy success.
P-72. Infection of the Reproductive Tract by Orchiepididymitis: Case Report
R. A. C. Monteiro1, J. R. Pariz1,2,3, H. E. Chemes4, J. Hallak1,2,3
1Laboratório Androscience, SP-SP
2Setor de Andrologia, Departamento de Urologia da FMUSP, SP-SP;
3Unidade de Toxicologia Reprodutiva, Departamento de Patologia da FMUSP, SP-SP
4Centro de Investigações Endocrinológicas, CEDIE-CONICET, Buenos Aires, Argentina
INTRODUCTION: Male reproductive tract infections are often associated with reduced fertile potential, mainly changing the sperm motility parameters.
CASE REPORT: Patient 29 years, bilateral varicocele, is referred for treatment 2 years of primary infertility. In the first semen analysis showed a concentration of 129x106 sperm/ml. It was referred to varicocelectomy with bilateral testicular biopsy, and presented Copenhagen index Modified 1.1.1.0, normal spermatogenesis. After surgery, hCG + r-FSH was administered, resulting in an increase in sperm concentration (134 x106 sperm/ml) and leukocytospermia (2.4 million cells/ml). Vibramycin and tetracycline was administered. The ICSI was performed after 90 days, with successful pregnancies.
Two years later, seminal analysis was performed, which showed concentration 1.2x106 sperm/ml, negative Endtz test, and culture positive for E. coli and Enterococcus spp, featuring an infection of the reproductive tract.
Acute orchiepididymitis. Tetracycline was administered orall for 6 days and return of the hormonal treatment. It was observed after treatment no culture of bacterial flora and increased concentration to 10.0x106 sperm/ml.
Three more ICSI attempts were unsuccessfully made. Was performed ultrastructural analysis of sperm morphology, which showed severe increase of sperm with maturation and changes in chromatin compaction it was requested. In the face of psychological research, the patient showed symptoms of stress and depression after unsuccessful pregnancy attempts.
The hypothesis of receptor depletion for r-hCG and FSH were analyzed and the need for its recovery interval for a new phase of hormonal induction was seen.
COMMENTS: Bacterial diseases of genitourinary tract, as they are asymptomatic, require proper clinical management, because the rate of occurrence in men in fertile age is high.
The fall of concentration and motility of the patient is evident after infection by E. coli and Enterococcus spp., with ultrastructural damage compression and maturation of sperm chromatin. Therefore, we suggest that bacterial infection may be a factor affecting male fertility and should be included in the evaluation of couples in assisted reproduction treatment.
P-73. Oocytes Vitrification to Maintain the Female Fertility: A Trend Growing in Patients Ever Younger
C. G. Basso1; N. P. de Oliveira1, C. G. Dutra1; F. Robi1, N. Frantz1
1Nilo Frantz Centro de Reprodução Humana – Porto Alegre - Brasil
OBJECTIVE: To evaluate whether there is increasing awareness of the female population about the importance of age in the successful preservation of gametes, causing them to seek this service getting younger.
MATERIAL AND METHODS: Specific cycles of oocyte vitrification for social preservation of fertility were selected conducted in the years 2012, 2013 and 2014. We assessed the number of annual cycles and the average age of patients who underwent the procedure. Later cases were divided into four age categories: 20-29 years, 30-34 years, 35-40 years and 40 years or more. The number of cases per year and also within each age group was recorded.
RESULTS: There was a growing number of fertility preservation cases from 2012 to 2014 and a decrease in age of patients seeking this treatment. In 2012 the average age was 35.5 years in 2013 to 35.2 years in 2014 and 33.8 years. When assessing cases within the age groups, there was an increase in demand for the procedure in younger categories, associated with the reduction in older ages. In 2012, there was greater demand for cases in patients of 35-39 years (63% of cases), the following year that number dropped to 55% of cases still being observed an increase of 18% in demand of the procedure in patients 30- 34 years. Already in 2014, again we observed decline in cases where patients 35-39 years (43%) and increased demand in younger patients (39% in patients 30-34 years).
CONCLUSIONS: We conclude that although there is still some resistance from patients to seek specialized services in assisted reproduction for cryopreservation of gametes, this demand has been occurring earlier in the last three years. Women who wish to postpone motherhood today have greater clarification and technology available to use the cryopreservation methods, although still is necessary further awareness that age is an important factor for better
results.