JBRA Assist. Reprod. 2016;20 (3):168-193
POSTER PRESENTATIONS
doi: 10.5935/1518-0557.20160036
Abstracts of the 20th Annual Congress of the SBRA, Belo Horizonte/MG 14-17 September 2016
P-01. Folliculogenesis progression in ectopic grafted ovarians after vitrification and devitrification followed by exogenous stimulation
Thalys J M Alves1, Marco T Dias1, Filipe P Barreto1, Jhéssica L M Gonzaga1, Paulo H A Campos-Júnior1
1Universidade Federal de São João del Rei/MG, Brazil
Objective: The aim of this study was to evaluate the folliculogenesis progression in mice ovaries after vitrification/devitrification followed by ectopic autotransplantation.
Methods: Female Balbc mice (60days, n=12), were anesthetized and bilaterally ovariectomized. One ovary was kept in buffer (PBS) during the procedure (control group – fresh). The other ovary was placed in PBS and then vitrified/devitrified using the IngáMed® kits, following the manufacturer’s instructions. Both ovaries were subcutaneously transplanted and after 21 days some animals (n=6) received 5UI of eCG (equine chorionic gonadotropin, Novormon 5000®) and, after 48h, 5UI of hCG (human chorionic gonadotropin, Vetecor®), analogous to FSH and LH respectively; other animals received PBS (n=6; control). Three days later, the hosts were euthanized and grafts were recovered, processed to histology (HE) and qualitatively analyzed.
Results: Primordial, primary, multilaminar and antral follicles were observed in fresh ovaries, with or without hormonal stimulation. In vitrified/devitrified tissues without stimulation, folliculogenesis were observed up to the multilaminar stage and in those with exogenous stimulation, a higher follicular density was observed, with follicles in preovulatory stage. Atretic follicles also were observed in all groups.
Conclusions: Folliculogenesis progression was observed in fresh and vitrified tissues; however, hormonal superstimulation using exogenous gonadotropins brought better results. This study showed, for the first time in the literature, the feasibility of the ovarian tissue vitrification technique, without morpho- functional damages. So, this technique could be used for fertility preservation and should be more investigated.
P-02. Efficiency of vitrification-warming blastocyst transfer in regular patients, egg donation program and embryo biopsy cycles: 1.5 years of experience with Ingamed® protocol
Mariana N Barreto1, Bruna Barros1, Eduardo L A da Motta1, Paulo C Serafini1, Tatiana C S Bonetti1, Jose R Alegretti1
1Huntington Medicina Reprodutiva, Sao Paulo/SP, Brazil
Objective: With the improvement of cryopreservation techniques, the vitrificationwarmed embryo transfers have been a common practice in IVF cycles. The aim of this study was to describe the efficiency of vitrified-warmed embryos transfer for regular patients, egg donation program and biopsied embryos.
Methods: Data from 786 cryopreserved blastocyst transfers cycles from January/2015 to March/2016 in a private IVF clinic were retrospectively analyzed. Vitrification used an open system pallet and Ingamed® media protocol. All patients performed vitrifiedwarmed blastocyst after endometrium preparation. Patients were split into three groups: regular patients submitted to frozen embryo transfer (FET, n=422), patients undergoing oocyte donation program (ODP) and FET (FET-ODP), n=144) and patients that had their embryos biopsied before freezing for preimplantation genetic diagnosis (PGD) and subsequent FET (FET-PGD, n=220).
Results: Women ages in the study groups were: FET: 34.6±3.9, FET-ODP: 41.9±5.2 and FET-PGD: 36.5±3.7 years. Blastocyst survival rate after warming were 96.9%, 98.8% and 98.6%, and the number of blastocyst transferred were 2.0±0.5, 2.0±0.6 and 1.5±0.5 for FET, FET-OR and FET-PGD, respectively. Clinical pregnancy rates were FET: 49.1%, FETODP: 54.2% and FET-PGD: 50.9%.
Conclusions: The literature shows the cryopreserved embryo transfers present improved clinical outcomes due to better condition of endometrium and embryo sincronization, corroborating our findings. The experience with open system pallet and Ingamed® media protocol resulted in clinical pregnancy rate of at least 50% independent of patient profile, suggesting the effectivity and safety procedure for regular IVF clinical practice.
P-03. Evaluation of biochemical and reproductive parameters of rats submitted to administration of commercial energy drink
Eduardo S de Araújo1, David Schaefer1, Anna E A do Nascimento1, Rafael A Salvador1, Alfred Senn2, David Til1, Marcel Frajblat3, Vera Lucia L Amaral1
1Universidade do Vale do Itajai-UNIVALI, Itajai/SC, Brazil
2Fondation pour l’Andrologie, la Biologie et l’Endocrinologie de la Reproduction - FABER - Lausanne, Switzerland
3Universidade Federal do Rio de Janeiro-UFRJ/RJ, Brazil
Objective: To evaluate the effect of commercial energy drink on biochemical and reproductive parameters in rats.
Methods: Male Wistar rats (n=40) adults were treated for 120 days with energy drink, to cover two Spermatogenesis cycles. Animals were divided into 4 groups: control group (CTRL) received only water. Energy dring for the other groups were calculated by allometric extrapolation (values per animal, 250g): DT - 2,36mL (therapeutic dose); D3 - 7,47mL (3x therapeutic dose) and D6 - 14,16mL (6x therapeutic dose). Signs of toxicity, body weight and organ, reproductive parameters (motility, concentration and morphology) and biochemical markers of liver function, kidney and heart (alanine aminotransferase, aspartate aminotransferase, alkaline phosphatase, lactate dehydrogenase, urea, creatinine, creatine phosphokinase, creatine kinase MB fraction), and the total testosterone hormone were evaluated.
Results: There was a decrease (P <0.05) in concentration of spermatozoa in the treated groups (DT - 8.5 ± 0.67; D3 - 7.2 ± 0.90; D6 - 8.4 ± 0.90) compared with control (12.3 ± 1.18). However there was no difference in the weight of the organs, toxicity, biochemical markers and other sperm parameters (motility and morphology).
Conclusions: Energy drinks, when consumed for long periods and at high concentrations, may negatively interfere with sperm concentration in rats.
P-04. Pregnancy outcome after Day 3 embryo transfer versus blastocyst stage transfer in patients under 35 years
João Paolo Bilibio1,2, Jessica Barros2, Juscelino Saba Junior2, Fabio Nascimento1, Bruno B da Silva1, Yasmin Maciel2, Panila L Lorenzzoni1, Jenny S L Afonso2, Arivaldo Meireles1
1Clínica PRONATUS - Medicina Reprodutiva, Belém/ PA, Brazil
2UFPA - Universidade Federal do Pará, Brazil
Objetive: Determine if blastocyst stage embryo transfers improve the chance of pregnancy and decrease abortion in patients less than 35 year compared with cleavage stage (Day 3).
Methods: The setting for this study was a fertility center, a case control study was performed with 149 women under 35 years undergoing IVF treatments using r- FSH and recombinant GnRH antagonist protocol. All the study subjects underwent controlled ovarian stimulation using r- FSH and recombinant GnRH antagonist protocol and were into two groups : D3 transfer (D3 group n= 74) and blastocyst transfer (D5 group n=75). Ongoing pregnancies, miscarriage, implantation rate were evaluated.
Results: The mean age were 31.6 years (D3 group) versus 32.14 years (D5 group) (years), P 0.121. Mean infertility time were 4.1 years (D3 Group) versus 4.3 years (D5 group), P 0.776). The mean of oocyte MII collected were 9.45 ( D3 group) versus 9.45 (D5 group), P 0.142. The pregnancy rate were 58.1% (D3 group) versus 57.1 (D5 group), P 0.917. The miscarriage rate were 16.9% (D3 group) versus 28.5% (D5 group), P 0.248. We did not find any difference in the number of antral follicles, the values of FSH, LH and estradiol on the third day of the cycle, the values of FSH, LH and estradiol on the day of hCG and endometrial thickness in both groups.
Conclusions: Improve laboratory standards and better culture media have media extended culture to blastocyst stage a reality to identify embryos with maximum implantation potential. However the observed pregnancy rate and abortion rate were similar between the two groups (D3 versus blastocyst) in patients under 35 years. The observed pregnancy rate do not allow us to take a position in favor of blastocyst or day 3 transfer in patients under 35 years.
P-05. Effect of endometrioma cysts on embryo quality and fertilization rate after IVF/ICSI
Yanna A R de Lima1, Fabiana C Approbato1, Mônica C S Maia1, Marisa S Ramos1, Maria Z P Brito1, Elisete N Santos1, Iulla A da Silveira1, Mário S Approbato1
1Laboratório de Reprodução Humana, Hospital das Clínicas, Universidade Federal de Goiás/GO, Brazil
Objective: Endometrioma cysts have been associated with poor outcomes related to assisted human reproduction procedures. This study aimed to evaluate the effect of endometriomas on embrio fragmentation (Depa-Martynow et al., 2007) and oocytes fertilization among women performing IVF/ICSI.
Methods: A case-control study was performed. The population comprised women with diagnosis of endometriosis, with or without endometrioma cysts, presenting to IVF/ICSI procedures. Risk (Odds Ratio – OR) of endometrioma to generate fragmented embryos (B/C/D) or to affect fertilization rates was calculated by Chi-square test using Epi Info software.
Results: A total of 781 patients cases were retrieved from medical files. Endometrioma cysts were observed among 31 women (31/781, 4%). Oocytes were retrieved in 23 out of 31 (74.2%) women with endometrioma and in 639 out of 750 (85.2%) women without endometrioma. Regarding oocyte fertilization rates, there was no significant difference among both groups (Fig1). However, the no endometrioma group presented significant less embryos with fragmentation at day 3 than the other group (OR=9.557; CI95%: 1.342-68.051; P<0.001) Fig 2.
Conclusions: Although endometrioma cysts were not associated with oocyte fertilization, it may interfere at embryo fragmentation at day 3. However, more studies are needed to confirm this hypothesis.
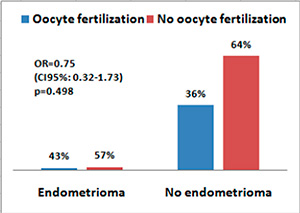
Figure 1. Oocyte fertilization rate among women with and without endometrioma.
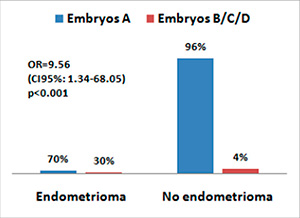
Figure 2. Distribution of embryo fragmentation among women with and without endometrioma.
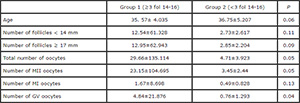
P-06. Evaluation of oocyte profile of patients undergoing controlled ovarian stimulation (COS) with Elonva®
José A L Neto1, Ana P Peixoto1, Alessandro Schuffner1, Vinicius B da Rosa1
1Clínica Conceber - Centro de Medicina Reprodutiva, Curitiba/ PR, Brazil
Objective: EOC Effectiveness using Elonva® by assessing the oocyte profile.
Methods: A retrospective study of case-control with 231 EOC cycles from 168 patients between May 2015 and May 2016. Cycles were divided between groups Elonva® (n=95) and control (n=136). The pituitary suppression of groups was made with GnRH antagonist. The Elonva® patients received single doses of 100 or 150 micrograms associated with additional ovarian stimulation with rFSH or hMG. Control patients received daily doses of rFSH or hMG. It was evaluated: endometrial thickness on the day of hCG; number of follicles over 12mm, oocytes retrieved, M2 oocytes and fertilized oocytes. Statistical analysis was performed using ANOVA.
Results: The Elonva® and control groups were similar for age (36.7±0.6 and 36.4±0.4, P=0.68), BMI (23.7±0.4 and 24.1±0.4, P=0.46), hCG administration day (11.9±0.4 and 11.3±0.2, P=0.36), AMH (2±0.3 and 2.4±0.6, P=0.55) and number of oocytes injected (5.6±0.4 and 5.7±0.4, P=0.89). The groups showed no significant differences for the parameters: endometrial thickness (9.1±0.2 and 8.9±0.2, P=0.45), number of follicles (9.2±0.7 and 8.9±0.5, P=0.71), number of oocytes (8.3±0.8 and 7.8±0.6, P=0.57), number of M2 (6.3±0.6 and 5.8±0.5, P=0.48), fertilized oocytes (3.5±0.3 and 3.6±0.3, P=0.94).
Conclusions: We conclude that the Elonva® and Control groups did not differ in any parameters evaluated in this study. Although the necessity of more studies to confirm these results, the Elonva® seems to be an option for ART patients with the benefit of the single application during the first week of stimulation.
P-07. Serological evaluation of Zika virus, in epidemic area, in asymptomatic infertility patients
Karina S A G Brandão1, Sofia A de Oliveira1, Gersia A Viana1, Manoela C L Lessa1, Valentina N C Muragaki1, Ana C M Trigo1, Pedro P B Filho1, Joaquim R C Lopes1
1CENAFERT - Centro de Medicina Reprodutiva, Salvador/BA, Brazil
Objectives: Descriptive analysis of the positive serology detection for Zika virus (IgM and IgG) in asymptomatic patients diagnosed with infertility. Materials and Material Methods: The study was conducted from March through May 2016 at the reproductive center. 134 patients were enrolled in this trial, 75 women and 54 men. Couples were starting in-vitro fertilization cycle with fresh or frozen egg/embryo and 21 women were doing cryopreservation oocytes. All of them had no symptoms of Zika virus (ZIKV) infection. Systematic screening was done to ZIKV, as recommended in rules of ANVISA, requesting IgG and IgM for women and IgM for men in epidemic area in Salvador, Bahia. Among the 134 patients, only 109 also carried out the analysis of the IgG fraction. It was used immunoassay technique (ELISA) to obtain the IgG fraction and the IgM serology was made with standard kit (Euroimmun®).
Results: All of the 134 samples, taken for IgM fraction analysis, were negative. In case of IgG fraction analysis, from the 109 collected samples, 51 were negative, 6 were indeterminate and 30 were positive (36% with suspected viral exposure). In this study, 18 women and 12 men had positive IgG ZIKV. In timely advice, these patients were advised to postpone treatment in 08 weeks and 06 months respectively.
Conclusions: More studies are necessary to corroborate the adoption of this practice, as it impacts on the security of time to begin assisted reproductive treatments.
P-08. High Progesterone levels at the initiation of stimulation cycles with antagonists and clinical pregnancy: still a concern?
Tatiana R Panaino1, Joyce B da Silva1, Maria A Tamm1, Paloma Lira1, Patricia C F Arêas1, Ana C A Mancebo1, Marcelo M de Souza1, Roberto A Antunes1, Maria Do Carmo B de Souza1
1Fertipraxis Centro de Reprodução Humana, Rio de Janeiro/ RJ, Brazil
Objective: Today most IVF/ICSI cycles use antagonists and the look of the experts turn to progesterone levels on the day of hCG injection. This study returns to assess the impact of serum progesterone at the initiation of stimulation and clinical pregnancy rates. This condition was previously suspected of decreased chance of pregnancy.
Methods: Retrospective cohort study including 610 fresh embryo transferred ICSI antagonist cycles from Jan 2004 to April 2015 in women ≤ 39 years. All of them were stimulated with rFSH, associated or not with HMG, and every patient had to get serum progesterone (P4) levels checked at the beginning of the ovarian stimulation. The ICSI cycles were divided in two groups according to the patient’s P4 level: ≤ 1500ng/dL or >1500ng/dL, based on the literature previous studies. The main outcome was clinical pregnancy.
Results: 568 patients fulfilled the inclusion criteria of the progesterone assay at the initiation of the cycle and had oocyte retrieval. There were 22 patients with P4 >1500ng/dL (3.9%) and 546 patients with P4 ≤ 1500ng/dL (96.1%). There was no difference in age, duration of stimulation and total amount of gonadotropins, but the number of oocytes retrieved was higher in the altered P4 group (10,81 ± 8,06 versus 7.93 ± 4.91, P = 0.009). However, no difference resulted in metaphase II oocytes, fertilization rate or number of embryos transferred (2.22 ± 0.75 versus 2.18 ± 0.73). In 7 out of these 22 altered P4 levels patients, the higher levels persisted on hCG day. There was no statistically significant difference in clinical pregnancy rates between groups (4/22= 18.2%) in P4 > 1500 versus (210/546 =38.4%) in P4 ≤ 1500. In the P4 group > 1500 from 4 pregnant women, one had a miscarriage.
Conclusions: No evidence can be attributed in the current study to elevated progesterone levels in the beginning of the cycles as a decreasing factor to pregnancy.
P-09. Ovarian grafts 10 days after xenotransplantation: folliculogenesis and recovery of viable oocytes
Marco T Dias1, Thalys J M Alves1, Fernanda E L Marinho1, Jhéssica L M Gonzaga1, Paulo H A Campos- Júnior1
1Universidade Federal de São João del Rei/MG, Brazil
Objective: Ovarian xenotransplantation is a promising alternative to preserve fertility of oncologic patients. However, several functional aspects of this procedure remained to be addressed. The aim of this study was evaluate the feasibility of xenotransplantation as a strategy to maintain ovarian grafts and produce oocytes.
Methods: Adult ovarian cortical pieces were xenotransplanted to the dorsal subcutaneous of female NOD-SCID mice (n=62). Grafts were recovered ten days after xenotransplantation. Host and graft weights; folliculogenesis progression; blood perfusion, relative gene expression and number of macrophage and neutrophil of xenografts; in vitro developmental competence of graft-derived oocytes were evaluated.
Results: Folliculogenesis was supported in the grafts. Primordial, primary, secondary, antral, and atretic follicles were observed. The xenografts showed a greater volumetric density of atretic follicles and higher hyperemia and number of host-derived macrophage and neutrophil (P<0.05), when compared to non-grafted fragments. There was a higher blood perfusion under the back skin in the transplantation sites of host animals than in control and non-grafted (P<0.01). BAX and PRDX1 genes were up-regulated, while BCL2, FSHR, IGF1R and IGF2R were down-regulated, when compared to the control (P<0.01). 27 oocytes were harvested from grafts, and some of these oocytes were able to give rise to blastocysts after IVF. However, cleavage and blastocyst rates of xenograft derived oocytes were lower than in control (P<0.01).
Conclusions: Despite showing some functional modifications, the ovarian xenografts were able to support folliculogenesis and produce functional oocytes that, for the first time in the literature, were able to give rise to blastocysts.
P-10. Ovarian vitrification does not affect the estradiol secretion and blood perfusion in autografted mice
Thalys J M Alves, Marco T Dias, Filipe P Barreto, Luiza A A C Pereira, Jhéssica L M Gonzaga, Paulo H A Campos-Júnior
1Universidade Federal de São João del Rei/MG, Brazil
Objective: Evaluate the estradiol levels and estrous cycle of fresh and vitrified ovarian autotransplant recipients as well the kinetics of graft blood perfusion.
Methods: Female Balbc mice (60days, n=24), were subdivided in: control, ovariectomized, autotransplanted with (C) fresh, and (D) vitrified ovaries, using IngáMed® kit. 24d after autotransplantation animals were euthanized, blood samples were collected and plasmatic estradiol levels were evaluated. Once a day, the estrous cycle stage was evaluated using vaginal smear. Furthermore, blood perfusion was evaluated 1, 5, 8, 12, 15, 19, 21 and 23 days after autotransplantation. The graft perfusion was estimated by the values obtained in the site of transplantation minus non-recipients skin. Data were analyzed using Neuman Keus test.
Results: Estradiol levels of vitrified and fresh ovary recipients were not statistically different (17.2pg/ml-1 and 18.3pg/ml-1 , respectively), however it was lower than control (22.3pg/ml-1 ) and higher than the ovariectomized (10.3pg/ml-1 ). Corroborating these findings, the analysis of the estrous cycle showed that graft recipients have stage frequency differences from the ovariectomized animals (proestrous 10.9% vs 0.0%, estrous 56.3% vs 0.0%, metaestrous 18.1% vs 13.3% and diestrous 14.5% vs 86.6% respectively). Additionally, the blood perfusion in the site of the transplantation was not different between fresh and vitrified groups and among all time points evaluated.
Conclusions: This study showed that ovarian grafts were (i) healthily received by the recipient mice (ii) able to produce estradiol that could (iii) restore the estrous cycle of those animals, and that the grafts were (iv) satisfactorily perfused since the transplantation.
P-11. Differential profile of transcripts in eutopic endometrium of infertile women with endometriosis and controls during the implantation window
Michele G da Broi1, Carlos V Rocha Jr1, Jessica R Plaça2,3, Kamila C Peronni2,3, Juliana Meola1, Wilson A Silva Jr2,3, Rui A Ferriani1, Paula A S Navarro1
1Human Reproduction Division, Department of Obstetrics and Gynecology, Ribeirão Preto School of Medicine, University of São Paulo, Ribeirão Preto, SP, Brazil
2Department of Genetics, Ribeirão Preto School of Medicine, University of São Paulo
3Center for Medical Genomics - HCFMRP/USP
Objective: Eutopic endometrium (EE) may be molecularly altered in infertile women with endometriosis. However, no study to date investigated the endometrial differential profile of all transcripts in these patients. This study aimed to evaluate by RNA-Seq all transcripts differentially expressed in EE of infertile women with endometriosis and controls during the implantation window (IW).
Methods: We performed a prospective case-control study. Endometrial biopsies were collected during the IW (confirmed by histological dating) from 6 infertile patients with endometriosis (3 endometriosis I/II, 3 endometriosis III/IV), 6 infertile controls and 5 fertile controls. RNA-Seq was performed using Illumina platform HISEQ2500, High Output, pairedend.
Results: We did not identify any differentially expressed genes (DEG) between infertile and fertile control groups and between endometriosis (with no regard to disease’s stage) and fertile control groups. However, five DEG (SCUBE1, CCL20, LGALS9C, TRIM29 and WNT11) were identified in the endometriosis III/IV, and 1 (KANSL1-AS1) in the endometriosis I/II groups compared to fertile controls. Two DEG (KANSL1-AS1 and VGLL3) were identified by comparing the endometriosis I/II group with the endometriosis III/IV group. Most of DEG are involved in biological processes of cell proliferation, vascularization, immune/inflammatory response, cell fate and chemokine/cytokines signaling.
Conclusions: The EE from infertile women with endometriosis, with no regard to disease’s stage, is molecularly similar to that from fertile controls in the IW. However, the subdivision of endometriosis into disease’s stages suggests molecular differences, especially in advanced disease. Future studies are necessary to investigate these deregulated genes in the different endometriosis’ stages.
P-12. Transfer of vitrified embryos after estrogen administration or in ovulatory cycles
Leonardo A M de Moraes1, Luciana P T de Aguiar1, Gabriella G de Oliveira1, Felipe D Silva1, Erika M Brescia1, Camila O S Caires1
1Clinica Fertibaby, Belo Horizonte/ MG, Brazil
Objective: to compare implantation and pregnancy rates after vitrified embryo transfers performed in cycles whose endometrium was prepared by estrogen administration or in cycles whose embryos were transferred after ovulation.
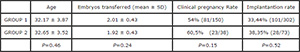
Methods: a total of 188 vitrified embryo transfers in patients under 38 years of age performed between January 2015 and April 2016 were analyzed. In group 1, the endometrium was prepared by oral or transdermal estrogen administration and by progesterone administered vaginally. In group 2, HCG was administered in the presence of a dominant follicle with a mean diameter between 17 and 20 mm and dydrogesterone was administered orally from the day after ovulation. Medications were continued until 12 weeks of pregnancy in both groups.
Results:
Conclusions: vitrified embryo transfers performed using HCG for follicular rupture and dydrogesterone orally from the day after ovulation had similar implantation and pregnancy rates when compared to cycles whose endometrial was prepared by estrogen administration.
P-13. Children of donated gametes: tell or not to tell?
Bruna R de Marchi1, Cássio L Fácio1, Ligiane A M de Paula1, Ligia F Previato1, Edilberto Araujo Filho1
1Centro de Reprodução Humana de São José do Preto (CRH-Rio Preto), São José do Rio Preto, SP, Brasil
Objective: Investigate disclosure decision of couples undergoing assisted human reproduction, through gamete donation, to their children about their conception. Methods: Total of 31 patients was evaluated, 26 undergoing in vitro fertilization and 5 intrauterine inseminations. Specific questionnaire was applied by telephone.
Results: Of 31 patients, 11 used donor oocytes (DO) and 20 donor sperm (DS). Twenty-six heterosexual couples, 2 singles, and 3 female homosexual couples. Six had miscarriages, 1 died and 2 did not participate. Twenty-two answered the questionnaire. Results obtained: 12 heterosexual patients will not tell and reasons were: fear, conflicts (3: DO); just do not intend to tell, fear, fear of the child want to know who is the donor, fear of the child to feel strange, world chauvinistic and fear of prejudice (9: DS). Six patients that will tell them, but not yet told because: child is very young (1 heterosexual: DO); afraid, child young, (3 homosexual and 2 singles: DS). Four heterosexual patients do not know whether will tell: child very young, fear; regret, conflicts and shame (2: DO); fear of conflicts and child very young (2: DS). One patient repented and has doubt if will tell due afraid of conflicts, and she feels ashamed by inability to have a child with her own gametes.
Conclusions: Telling or not, 21 patients were satisfied with results encouraging others to make treatment with gamete donation if no other option exists. Repentant patient suggests psychological support to help patients before, during and after treatment by gamete donation.
P-14. Cryopreservation of human semen in medium TEST-yolk buffer or synthetic medium supplemented with phospholipid and antioxidant: Non-inferiority clinical trial
Aline Bomfim Silva1, Fernanda Sicchieri1, Alessandra A Vireque2, Marilda H Y Dantas1, Carlos A F Molina1, Rosana M dos Reis1
1Faculdade de Medicina de Ribeirão Preto, Universidade de São Paulo (FMRP-USP)
2Invitra Tecnologia da Reprodução Assistida
Objective: To determine the effectiveness of a synthetic cryoprotectant medium based on co-supplementation with phospholipids (PL) and antioxidants (ANTIOX-PL), compared to conventional TEST-yolk buffer containing chicken egg yolk in its formulation (TYB, Irvine Scientific), with respect to the sperm progressive motility (PR) and DNA fragmentation index (DFI).
Methods: Randomized study that included men aged 18 and 50, with semen volume ≥ 1.5 mL, concentration of spermatozoa ≥ 15x106 /mL and progressive motility ≥ 32%. Samples of 43 patients, divided into two aliquots with equal volumes, were randomly allocated to two groups: ANTIOX-PL and TYB. The PR motility and DFI in sperm cells were evaluated before freezing and after thawing. The evaluation of outcomes was blinded to group assignment. Recruitment is still underway.
Results: PR motility (P=0.23) and DFI in spermatozoa (P=0.28) cryopreserved with medium ANTIOX-PL showed no difference compared to the TYB.
Conclusions: The ANTIOX-PL medium can be considered no less efficacious than the conventional TEST-yolk buffer relative to sperm PR motility and DNA fragmentation parameters, and offers important advantages as a defined chemical composition which identifies the added components and information about their mechanisms of action in the cell, a longer period of shelf-life which facilitates a free of degradation storage and reduces the risk of microbiological contamination due to the absence of animal additives, and better quality control procedures for application in assisted human reproduction.
P-15. Embryo re-biopsy for failure DNA amplification diagnosis by aCGH
Monique B Bueno1
1Igenomix - laboratório de medicina genética, Sao Paulo/ SP, Brazil
Objective: To describe the euploidy and aneuploidy frequency present in re-biopsied embryos subjected to analysis by PGS, and define the importance of re-biopsy in routine of ART laboratories.
Methods: Retrospective analysis of 51 embryos from 32 cycles of ART, from April 2014 to March 2016. Embryos were previously biopsied and subjected to chromosomal analysis by Comparative Genomic Hybridization (aCGH), and analysis result obtained after DNA amplification was failure. Thus, the embryos were re-biopsied and subjected to analysis in order to diagnose them as euploid or aneuploid. From result of analysis, embryos diagnosed as euploid were divided into three sub-groups in accordance with maternal age, in order to investigate the correlation between maternal age and DNA amplification failure in embryos subjected to chromosomal analysis by aCGH.
Results: From total number of embryos subjected to re-biopsy and chromosome analysis, embryos were diagnosed as euploid (n=15/51), aneuploid (n=26/51) or had amplification failure (n=10/51). The frequency of aneuploid embryos was 51%, representing more than half of studied embryos. Embryos diagnosed as euploid which had failed DNA amplification, represented 29.4% and 19.6%, respectively. Embryos diagnosed as euploid were divided into subgroups ≤35 years, 36-39 years, ≥40 years and represented [n=8/15;n=6/15;n=1/15(53.3%; 40.0%; 6.7%)], respectively.
Conclusions: The results demonstrate the importance of re-biopsy and PGS in previously biopsied embryos chromosomally analyzed by aCGH, which had DNA amplification failure in first analysis. According to our data, re-biopsy may contribute positively to results in cycles of patients undergoing ART treatments, increasing the chances of getting a healthy pregnancy, regardless maternal age.
P-16. The use of social networks to inform women on endometriosis and infertility: preliminary results
Márcia M Carneiro1,2, Ana L L R Baroni2, Eduardo B Candido2, Agnaldo L da Silva Filho2, Márcia C F Ferreira1,2
1Centro de Reprodução Humana MATER DEI Belo Horizonte-MG, Brasil
2Departamento de Ginecologia e Obstetrícia Faculdade de Medicina da UFMG, Belo Horizonte-MG, Brasil
Objective: The quality of infertility information on the internet is poor. Social networking may be a valuable tool to educate and inform patients. We thus aimed at establishing a social network page and use it to provide reliable information on endometriosis and infertility.
Methods: The page was designed by the Endometriosis Multidisplinary Team at Federal University of Minas Gerais (UFMG) to inform about various aspects related to endometriosis including infertility. Topics were selected based on the most frequent doubts and misconceptions presented by women during consultation.
Results: The page went online on Facebook on April 21st 2016 and 72 posts have been published. There are currently 561 fans (82% women; 18% men), the majority are Brazilian (n=550) from Minas Gerais, buth there are people from all over Brazil, the United States and Europe. Posts have been seen by 12459 people, the majority being Brazilian women aged 25- 34 (42%) and 35-44(19%). Most viewed posts are related to the following topics: deep infilltrating endometriosis (n=4425 views); the use of intrauterine levonorgestrel system (3100 views); IVF and endometriosis? (2885 views); endometriosis and infertility (1290 views) and how to schedule an appointment 1264 views). The numbers keep increasing day after day.
Conclusions: We have sucessfully developed a Facebook page used by reproductive age men and women to obtain information related to endometriosis and infertility. The development of pages with reliable information is an important tool to inform men and women and help them make informed choices on their fertility and available treatments.
P-17. Follicular flushing associated to oocyte retrieval in poor responders submitted to art increase the number of oocytes, embryos and pregnancy rates
Anna L M Souza1, Marcos Sampaio2, Selmo Geber 1,2, Graciele B Noronha1, Ludiana G R Coster1, Roberta S G de Oliveira1
1UFMG – Universidade Federal de Minas Gerais, Belo Horizonte/MG, Brazil
2ORIGEN – Center for Reproductive Medicine, Rio de Janeiro/RJ, Brazil
Objective: Follicular flushing during oocyte retrieval for ART treatment can be an alternative to increase the number of retrieved oocytes and optimize results in poor-responder women. However there is a lack of evidence of improvement in the results as the number of cases is still scarce. Evaluate the impact of follicular flushing in assisted reproductive cycles of poor responders.
Methods: Retrospective study of 524 cycles of 384 patients with poor ovarian response undergoing ICSI with follicular flushing .
Results: The mean age of the patients was 38.2 ± 4.2. The number of oocytes retrieved after flushing was significantly higher than those with no flushing (2.7±1.1 and 1.8±1.2 - P<0.001) with 31.8% of oocytes retrieved from flushing. There was also a significant correlation between MII, total number of embryos and pregnancy rate. When one MII oocyte was retrieved, pregnancy rate was 6.4%; for two MII, 20.8%; three MII, 22.0%; with four 39.6% (P<0.001). When one embryo was transferred, pregnancy rate was 12.6%; for two embryos 24.1%; for three embryos 28.1%, and four embryos, 33.3% (P=0.010).
Conclusions: Follicular flushing in poor-responder patients may be an alternative to increase the number of oocytes retrieved and consequently increase the pregnancy rate.
P-18. Preimplantation Genetic Diagnosis associated to Duchenne Muscular Dystrophy
Caio P Barbosa1, Camila M Trevisan1, Gabriel S Conceição1, Monise C Santos1, Denise M Christofolini1, Bianca Bianco1
1Centro de Reprodução e Genética - Faculdade de Medicina do ABC
Objective: Duchenne Muscular Dystrophy (DMD) is an X-linked recessive disease (Xp21.2) which occurs due to changes in the dystrophin gene. Deletions and duplications of one or more exons of gene are responsible for 65% of pathogenic mutations, and the others are point mutations. Most of the mutations cause progressive and irreversible degeneration of muscles. Usually weakness in the pelvic girdle muscles arises in the first five years old and disease leads to death around the 2nd decade from heart or respiratory compromise. It affects 1:3,000 boys.
Methods: EPR, 38y, symptomatic patient heterozygous for a 2 to 47 exon mutation in DMD gene and GTS, 39y, sought genetic counseling service in 2014 to know about the Preimplantation Genetic Diagnosis (PGD), because they had a 6 year old son with DMD who died in 2012. They undergone four cycles of ICSI using 200UI FSHr protocol for controlled ovarian hyperstimulation. Eight D5/D6 embryos biopsies were analyzed by PCR for specific mutation analysis, followed by CGH array for aneuploidy analysis.
Results: PGD disclosed that two embryos had inherited the maternal DMD mutation, one embryo had chromosomal alteration and five embryos were normal. One blastocyst was transferred and resulted in a pregnancy. The child was a female, born after 38 gestational weeks by cesarean section, with 2970g of weight and 43cm height. The other embryos remain vitrified.
Conclusions: Embryo analysis using the associated techniques of PCR and CGH array showed to be safe for embryo selection in cases of X-linked disorders, as DMD. Keywords: Duchenne Muscular Dystrophy, PCR, CGH array, PGD.
P-19. Ovarian tissue bovine cryopreservation associated with in vitro folicular maturation in three-dimensional system to fertility preservation purposes
Daiane L. Bulgarelli1, Jacira R. Campos2, Catieli G. Gervázio1, Luciene A. Batista1, Thais Higa1, Marina M. Machado1, Ana Carolina J. S. Rosa e Silva1
1Gynecologic and Obstetrics Department, School of Medicine of Ribeirão Preto, University of São Paulo
2Clínic Genics Medicina Reprodutiva e Genômica
Objective: Assess the development capacity of secondary follicles from cryopreserved ovarian tissue associated with follicular maturation in three-dimensional system to obtain antral follicle and mature oocytes to fertility preservation application.
Methods: Bovine ovaries were selected, cut into fragments of 3x3x 0.5 mm3 and vitrified with glycerol, ethylene glycol and synthetic polymers in a closed system. After warming, the secondary follicles were isolated, encapsulated in alginate (0.25%) and cultured individually in ALFA-MEM with 5ng/ml FSH for 15 days in 5% CO2 and 38.5°C for 15 days. Follicular development in vitro by long-term culture was evaluated.
Results: In fresh group (control) showed increased diameter in vitro over the 15 days of culture in relation to vitrified group (P=0.002). Survival rate was increased in fresh group (37%) then vitrified group (18%; P= 0.04). Antral cavity was no difference in both groups (11% fresh and 3% vitrified; P=0.23). No statistical difference were found in fresh group (74%) and vitrified (61%) of oocytes/COC total recovery (P=0.21), rate of oocyte normal morphology recovery (fresh 54%, 40% vitrified; P=0.37) and COC normal morphology recovery (fresh 65%, 70% vitrified; P=1.0). COC submitted to IVM (17% fresh and 10% vitrified; P=1.0). Oocyte diameter decreased after IVM in both groups, only immature oocytes were obtained.
Conclusions: Secondary follicles vitrified in situ and in vitro matured in three-dimensional system were able to development to antral stage, However, only immature oocytes were obtained. More studies are necessary to improve the protocols used.
P-20. Blastocyst morphology affects the implantation rate in euploid embryo transfers
Marcos I R Kulmann1, Marcos Hoher1, Carla G Basso1, Norma P de Oliveira1, Gerta N Frantz1, Caroline G Dutra1, Adriana Bos-Mikich1, Nilo Frantz1
1Centro de Reprodução Humana Nilo Frantz - Porto Alegre/RS, Brasil
Objective: Assess the relationship between blastocyst morphology and euplody rate (ER) as well as verify how the morphology affects the implantation rate (IR) in single thawed euploid embryo transfer (STEET).
Methods: This is a retrospective study from 194 embryos that underwent PGS (a-CGH or NGS) after trophectoderm (TE) biopsy in D5 or D6 and from 49 cycles involving STEET between 2014 and 2016. The blastocyst quality was defined according to the Gardner and Schoolcraft criteria. Two groups were categorized for ER and IR assessment: top (AA, AB and BA) and average/poor (BB, BC, CB and CC) quality. Inner cell mass (ICM) and TE scores were also independently analyzed. Student’s t-test and Fisher’s exact test were used to analyze the results, considering P<0.05 as statistically different.
Results: We observed that both ER and IR were associated with blastocyst morphology. The ER was 68,75% and 45,38% (P=0,0023) for top and average/poor quality groups. The IR was 61,11% and 25,92% (P=0,0296), respectively. Besides, the data showed that separately assessment of ICM or TE scores had no effect on IR. Finally, there is no difference concerning age, body mass index and endometrium thickness between the groups.
Conclusions: The blastocyst morphology seems to be an important factor to select the most suitable embryo for STEET. For this purpose, ICM and TE good scores are required to achieve the highest implantation rate possible.
P-21. The chemokine receptor-2 (CCR2) and its ligand, CCL2 is expressed in oocytes and oviduct epithelium, respectively and can be related to oocyte transport
Alana G A Santos1, Luiza A A C Pereira1, Natália L C Ciriaco1, Remo C Russo2, Paulo H A Campos-Junior1
1Laboratório de Morfofisiologia e Biotecnologia Gonadal - Universidade Federal de São João del Rei/MG, Brazil
2Laboratório de Imunologia e Mecânica Pulmonar - Universidade Federal de Minas Gerais, Brazil
Objective: Chemokines are cytokines characterized by their chemotactic function. Previously, we showed that CCR2 is expressed in growing follicles and that CCR2 deficiency alters follicular mobilization. The aim of this study wasinvestigate the expression of CCR2 and CCL2 in ovulated oocytes and oviduct of wild type mice (WT), as well the fertility of WT and CCR2-/-.
Methods: Oocytes and oviducts were collected from female (60 days-old) WT (n=10) and CCR2-/- (n=10) mice. The immunolocalization of CCR2 and CCL2 in ovulated oocytes and oviducts of WT were performed using standardized protocol and these structures were analyzed in confocal microscope. The estrous cycle length of WT and CCR2-/- were determined by vaginal smears (for 16 days). The number of ovulated oocytes after gonadotropin stimulation was also investigated.
Results: CCR2 was observed on denuded oocyte membrane and the granulosa cells of cumulus- oocyte complexes. CCL2 was observed just on the oviduct epithelial cells. CCR2-/- showed anlonger estrous cycle compared to WT (5.5±0.6vs 7.2±0.8, respectively). However, the number of ovulated oocytes were not different (13±4.15 CCR2-/-vs9±2.49 WT; P<0.05).
Conclusions: Our studies suggest that CCR2 playsa role in ovarian homeostasis. The longer duration of estrous cycle found in CCR2-/- can slow down the depletion of ovarian follicular reserve and can lead to a femalefertile prolonging. In addition, CCR2 expression observed in ovulated oocyte-cumulus complex and immunolocalization of its ligand in the epithelium of the uterine tube also suggest that this receptor-ligand interaction could be influence the oocyte transport.
P-22. Seminal parameters after different standard methods of sperm selection: comparisons between two techniques
Franciele O Lunardi1, João E Pinheiro Neto1, Lilian M C Serio1, Benner G Alves2, Kele A Alves2, Maria C Cardoso3, Luciana P T de Aguiar4, Leonardo A M de Moraes4, Daniel P D de Paula1
1Fertibaby Ceará, Fortaleza/CE, Brazil
2Universidade Estadual do Ceará, Brazil
3Centro de Fertilidade Vida, Rio de Janeiro/RJ, Brazil
4Fertibaby Medicina Reprodutiva, Belo Horizonte/MG, Brazil
Objective: Seminal parameters are associated with success rates in assisted reproduction procedures. The main sperm processing methods are upward migration - Swim up (SU) and the discontinuous gradient (DG). The first, SU, is based on the migration of sperm with higher motility toward clean medium genteelly layered on the top of a volume of semen or a pellet of seminal cells after centrifugation. The DG method is based on the separation by centrifugation of the semen through different density gradients. Both techniques separate rapid gametes from immobile sperm and non-cellular elements of semen. The seminal parameters have not been systematically compared after these two methods. Therefore, the aim of this work was to compare the methods SU and centrifugation through DG to evaluate the improvement of sperm parameters.
Methods: The semen samples (n = 30) were obtained after signing consent and equally divided to be processed by SU and DG methods. Next, the fresh and processed samples were analyzed for parameters as concentration, motility (types A, B, C and D), morphology (according to Kruger and World Health Organization-WHO), acrosome index, teratozoospermia index and sperm deformity index.
Results: After processing by both methods, the sperm concentration decreased significantly compared to the fresh sample (26.4 ± 3.5 million / ml). The sperm recovery rate was greater for DG compared to SU method (15.7 ± 2.7 million / ml vs 5.5 ± 0.8 million/ml). Regarding the motility rates type A and B, both methods were similar and higher (P <0.05) than the unprocessed semen . However, DG method had higher amount (P <0.05) of low sperm motility or zero motility (types C and D). The seminal parameters for assessing the morphology (Kruger and WHO), acrosomal index, teratozoospermia index and sperm deformity index were similar in between both methods of semen processing, but improved significantly (P <0.05) when compared to fresh samples.
Conclusions: the SU and DG methods were effective in selecting a larger population of morphologically normal cells. Moreover, the DG method is more suitable to obtain samples with higher sperm concentrations and SU method is eligible for better quality in motility.
P-23. Endometrial Receptivity Analysis for implantation failure in IVF: findings and results
Edilberto Araujo Filho1, Cássio L Fácio1, Ligiane A M de Paula1, Ligia F Previato1
1Centro de Reprodução Humana de São José do Preto (CRH-Rio Preto), São José do Rio Preto/SP, Brazil
Objective: Investigate endometrial receptivity through Endometrial Receptivity Analysis (ERA) in patients with at least two in vitro fertilization (IVF) implantation failures.
Material and Methods: Nineteen patients were submitted to ERA, age range: 30-40 years. Endometrium preparation started on day 2 of the cycle after basal ultrasound showing uterus and ovaries unchanged. It was used estradiol, 6mg/day from days 2 to 8, then, ultrasound was performed to measure endometrium, to dose E2 and P4, and Doppler of uterine arteries. When endometrium thickness reached at least 8 mm (not before day 9 of replacement), estradiol ≥400pg/ml, 800 mg/day micronized progesterone (vaginal) (Utrogestan) was started, and biopsy for ERA was made on day 5 of Utrogestan. Cases of natural cycle, ultrasound was started on day 8 and when dominant follicle reached 18mm, ultrasound was performed daily. We dosed E2, Pg and LH daily. When LH increased, biopsy was performed on day + 7 of the LH range.
Results: Of 19 patients submitted to ERA, in 2 it was performed after a natural cycle, and 1 of them, the endometrium was post-receptive. The other 17, biopsy was performed in artificial cycle: 10 non-receptive; 1, test invalid; and 6 receptive. Among non-receptive: 9 pre-receptive and 1 post-receptive. Of 11 patients nonreceptive, 5 tried another IVF cycle and 3 are clinically pregnant. Conclusions: ERA seems to be an important tool in the evaluation of the endometrium in patients with recurrent IVF failure. Greater casuistic is necessary to confirm these findings.
P-24. Influence on the development of vitrified isolated secondary follicles after in vitro cultured in α-MEM and TCM base media in alginate matrix
Daiane L. Bulgarelli1, Jacira R. Campos2, Catieli G. Gervázio1, Luciene A. Batista1, Thais T. Higa1, Mary B. Zelinski3, Ana Carolina J.S. Rosa e Silva1
1Gynecologic and Obstetrics Department, School of Medicine of Ribeirão Preto, University of São Paulo
2Clínic Genics Medicina Reprodutiva e Genômica.
3Division of Reproductive & Developmental Sciences, Oregon National Primate Research Center, Oregon Health & Sciences University, Beaverton, Oregon, USA
Objective: To verify whether vitrified secondary follicle needs different base media (α- MEM or TCM) to development in vitro in matrix alginate for a long- period.
Methods: bovine ovaries were selected and secondary follicles were mechanically isolated from fresh ovarian tissue, vitrified and after warming, they were encapsulated in alginate (0.25%) and cultured individually in α-MEM or TCM with 5ng/ml FSH in 5% CO2 and 38.5°C for 15 days. Follicular development were evaluated.
Results: No difference was found on growth between follicles cultured in α-MEM and TCM (P=0.98). However, fresh follicles showed increased diameter in α-MEM group (P=0.0029). Survival rate was in fresh groups 57% α-MEM and 46% TCM. In vitrified groups were 33% α-MEM and 20% TCM (P<0.005). The antral formation was increased in α-MEM fresh group (26%) than TCM fresh group (11%; P=0.03). In vitrified groups was not found statistical difference (13% α-MEM and 12% TCM; P = 0.99). Morphologically normal oocyte recovery no difference was found between fresh group (38% TCM and 29% α-MEM; P=0.58) and vitrified (25% TCM and 17% α-MEM; P=0.73). Morphologically normal cumulus oocyte-complexes (COC) normal recovery was fresh groups 81% TCM and 84% α-MEM (P=1.0) and vitrified groups 53% TCM and 67% α-MEM (P=0.49). After in vitro maturation, in fresh and vitrified groups showed only immature oocytes.
Conclusions: development of vitrified secondary follicles were evaluated and there were no superiority through α-MEM relative to TCM in vitrified follicles, and only in the fresh group media α-MEM showed better results.
P-25. Predictors for oocyte recovery
Emily de Conto1,2, Frederico A Reis Brandão1, Vanessa K Genro2, Rita de Cassia B Chapon1,2, Daniela S da Silva2, Joao S da Cunha-Filho1,2
1UFRGS - Universidade Federal do Rio Grande do Sul, Porto Alegre/RS, Brazil
2Insemine - Centro de Reprodução Humana, Porto Alegre/ RS, Brazil
Objective: To establish which variables best predict the recovery of oocytes in metaphase II in cycles of assisted reproductive technology. Study variables: age, AMH (anti-Mullerian hormone), AFC (antral follicle count) and follicles size ≥ 17mm on the day of hCG test.
Methods: This study analyzed 940 cycles of IVF in which MII oocytes were recovered in a Human Reproduction Center of Porto Alegre/ Brazil. The statistical test performed was Spearman Correlation and linear regression using the statistical program SPSS Statistics 20. P value ≤ 0.05 was considered statistically significant.
Results: The mean age of patients was 35.1 ± 2.9 years, AMH averaged 3.3 ± 3.4 pmol/L, AFC 10.8 ± 5.8, number of follicles ≥ 17mm 3.9 ± 3.3, number of oocytes in metaphase II 4.7 ± 3.6. Analyzing the number of MII oocytes as the outcome, the correlation coefficient indicates that this variable is associated with age, AMH, AFC and follicles ≥ 17mm. However, when applying linear regression, the number of MII oocytes recovered in assisted reproduction cycle is associated just with the number of follicles ≥ 17mm size (P = 0.001). The other results were aged for P = 0.121, P = 0.068 for AFC and P = 0.253 for AMH.
Conclusions: The most important predictor of the amount of MII oocytes recovered in assisted reproduction cycles in patients younger than 40 years is the number of follicles with size ≥ 17mm on the day of hCG administration. Keywords: oocyte recovery, follicles ≥ 17mm size, MII oocytes
P-26. Effect of varicocelectomy on sperm DNA fragmentation, global DNA methylation, semen quality and hormonal parameters in man with varicocele
Viviane P Santana1, Cristiana L Miranda-Furtado1, Maria A C Vasconcelos1, Marilda H Y Dantas1, Carlos A F Molina2, Rosana M Reis1
1Department of Gynecology and Obstetrics, Ribeirao Preto Medical School, University of Sao Paulo, Ribeirao Preto/SP, Brazil
2Department of Surgery and Anatomy, Ribeirao Preto Medical School, University of Sao Paulo, Ribeirao Preto/SP, Brazil
Objetive: Varicocelectomy may improve the seminal parameters and the quality of genetic material in men with varicocele. We sought to verify the effect of varicocelectomy on semen quality, hormonal parameters, sperm DNA fragmentation (SDF) and global DNA methylation (SGDM) in patients with varicocele.
Methods: This is a randomized clinical trial study, comprising 19 men with varicocele, in which six underwent to surgery (A) and 13 has not passed the procedure (B), evaluated before and after nine months. A control group without varicocele was used for comparisons (n = 19). The sperm quality was assessed by spermogram, SDF by Halosperm G2® kit and SGDM by ELISA (Enzyme- Linked Immunosorbent Assay). A higher rate of SDF, low sperm concentration and progressive motility was observed in patients with varicocele compared with the controls (P<0.05).
Results: In varicocele group, the patients who underwent surgery had a decrease in SDF and an increase in sperm concentration compared to those who have not undergone the procedure (P<0.05). Increased prolactin and decreased total testosterone concentrations was observed in the men without surgery (P<0.05). The SGDM was not different between varicocele (A: 49.967% ± 30.38; B: 49.813% ± 25.82) and control group (64.660% ± 17.08), but the surgery seems to improve SGDMin varicocele group.
Conclusions: Varicocele may be related to a higher percentage of SDF and decrease in sperm quality and varicocelectomy seems to improve these characteristics and may be a treatment for these patients. Confirmation of these findings is important to determine the actual effect of varicocelectomy these patients.
P-27. The embryo flash position immediately after IFV cycles transfer and assisted reproduction results
Karina S A G Brandão1, Janaina J M Maciel1, Tassia S Leão1, Sofia A de Oliveira1, Joaquim R C Lopes1
1CENAFERT - Centro de Medicina Reprodutiva, Salvador/ BA, Brazil
Objective: Check if intracavitary embryonic deposit distance and air bubble image position has different rate of clinical pregnancy when evaluated immediately after embryo transfer.
Methods: This study was conducted from January 2009 through December 2014 at a reproductive center in northwest of Brazil. Were analyzed 548 embryo transfers. During transfer, measure of the distance traveled by the catheter was made and, immediately after embryo transfer, the position of air bubble image distance from uterine fundus. Clinical pregnancy rate was evaluated and compared between patients with catheter measurement ≥ 6 cm, and embryo flash position (air bubble) ≤ 1 cm from uterine fundus. It was used x 2 Fisher’s Test to do analysis.
Results: Among the 548 evaluated cases, 60.4% of the patients had deposited the embryo ≥6 cm deep and 73.5% had the bubble image ≤ 1cm from the uterine fundus. Among the patients who had embryo deposition in distance ≥ 6 cm (331), 126 had clinical pregnancy (38.06%) and in patients with distance < 6 cm was 38.7% (P = 0.928). Among patients who had bubble image ≤ 1cm, 169 (41.94%) had clinical pregnancy while 28.27% of patients with bubble with distance >1cm had clinical pregnancy (P = 0.004).
Conclusions: The air bubble image ≤ 1 cm from the uterine fundus, verified immediately after embryo transfer, relates to higher clinical pregnancy rate compared to greater distances.
P-28. Auto report of regularity of patient’s menstrual cycles. Medical history is very reliable to predict ovulation. A cross-sectional study
Reinaldo S A Sasaki1, Mário S Approbato1, Mônica C S Maia1, Eliamar A B Fleury1,2, Christiane R Giviziez1, Neuma Zanluchi3
1Human Reproduction Center- Department of Obstetrics and Gynecology Clinical Hospital - Goias Federal University – Goiânia – Goiás – Brazil
2Musical School and Scenic Arts/Goias Federal University
3Hospital de Doenças Tropicais
Objetive: Infertility of ovulatory cause can reach up to a quarter of infertility etiologies and one of the questions in the clinical history of the patient is about the self perception of the regularity of menstrual cycles. The aim of this study is to assess whether the information on menstrual regularity is consistent with the assessment of the presence or absence of ovulation.
Methods: cross-sectional study. The inclusion criteria were: patients with infertility for at least one year, complete examination of monitoring ovulation, aged between 18 and 38 years completed. The patients were divided into two paired groups: those who reported regular menstrual cycles and those who reported irregular cycles. In the ultrasonographic monitoring of the ovulation were identified those ovulated and those that did not ovulate and was applied Fischer’s test.
Results: among the 199 patients who reported having regular menstrual cycles, 113 proven ovulated in ultrasound monitoring cycle and 86 patients did not ovulate. Among the 29 patients who reported irregular cycle, 24 not ovulated at the cycle monitoring. The Fisher’s exact test was applied and the p found was significant.
Conclusions: the story of the patient in the clinical interview about the presence of regular or irregular menstruation correlates with the presence or absence of ovulation, it should be taken in consideration in the reasoning of the etiology of infertility. This report would be important to direct the diagnosis of ovulatory regularity of the patient.
P-29. Aneuploidy rates in embryos biopsied on days 5 or 6
Alice Tagliani-Ribeiro1, Ricardo Azambuja1
1Fertilitat - Centro de Medicina Reprodutiva, Porto Alegre/RS, Brasil
Objective: Comparison of aneuploidy rates in embryos biopsied on Day 5 or 6 after fertilization.
Methods: Forty eight patients were submitted to in vitro fertilization (IVF) with embryo biopsy and preimplantational genetics screening (PGS), during the period of 2012-2016. All genetic analysis was performed with comparative genomic hybridization (CGH) or new generation sequencing (NGS). The biopsy was performed either on day 5 or day 6, depending on the embryo development.
Results: Embryos from 29 patients were biopsied on Day 5, with an average age of 35.3 years. The biopsy on Day 6 was performed in 19 patients, with average age of 36.6 years. Overall 174 embryos were biopsied, with 127 on 5º dia of culture and 47 on the 6º day. The rate of aneuploidy embryos biopsied on day 5 were 66.9%; and the aneuplody rate in embryos biopsied on Day 6 were 72.3% (P: 0.6198).
Conclusions: Although the number of cycles analyzed is small, there was no statistical difference when the aneuploidy rates were compared in embryos biopsied on Day 5 or 6. Therefore, the biopsy on Day 6 seems to be a good option for those patients that do not have blastocyst embryos on Day 5.
P-30. Evaluation of pregnancy rate using two soft embryo transfer catheters
Juliana Polisseni1, Carolina M de Assunção1, Fernanda Polisseni1, Josélio V Rosa1, Jociane V S Oliveira1, Larissa M Coutinho1, João P J Caetano1
1Pró-Criar Medicina Reprodutiva, MG, Brazil
Objective: We compared the efficacy of two different soft catheters on total pregnancy rates in patients undergoing ICSI.
Methods: A retrospective study was performed at Clinical of Reproductive Medicine in Zona of Mata Mineira, from April 2015 to April 2016. A total of 158 patients of ICSI cycle undergoing fresh embryo transfer (ET) were evaluated: Friedman IVF catheter (N=125) and Sydney IVF catheter (N=39). Chi-square test (P<0.05) was used to compare the effect of the catheters on the pregnancy rates. Difference between mean of age and number of embryo transfer of groups were evaluated Student’s t test (P<0.05) as mean±SEM.
Results: The mean age of the patients in the Friedman IVF catheter group was 35.31±0.46 (range: 18-47) and in the Sydney IVF catheter group was 35.18±0.94 (range: 22-50). For number of embryo transfer, the result of Friedman IVF catheter was 2.28±0.07 and Sydney IVF catheter was 2.31±0.10. The total pregnancy rate was 44.8% (56/125) in Friedman IVF catheter and 43.6% (17/39) in Sydney IVF catheter. The difference was not significant (P>0.05) for age of patients, number of embryo transfer and total pregnancy rate between groups.
Conclusions: Our study suggests that use soft catheters Sydney or Friedman of embryo transfer do not affect the outcome of ART cycles. This study was important because ET is probably the most important procedures in assisted reproduction and choice of the catheter is also very important for a good prognosis after embryo transfer.
P-31. Ovarian tissue vitrification in prepubertal wistar rats: comparative analysis among different protocols
Leticia Wietcovsky1, Angélica Siewert1, Tamara Lamim1, David Til1, Rafael A Salvador1, Nicole L L Amaral2, Marcel Frajblat3, Vera L L Amaral1
1UNIVALI - Universidade do Vale do Itajaí, Itajai, SC, Brazil
2CCV - Centro Clínico Veterinário, Itajai/ SC, Brazil
3Universidade Federal do Rio de Janeiro – UFRJ, RJ, Brazil
Objective: Compare the efficiency of two ovarian tissue vitrification protocols in prepubertal Wistar rats.
Methods: Oophorectomy was performed in eight animals. Ovaries were divided in approximately in pieces of 1mm diameter. One of the pieces was dissected fresh and follicle viability was assessed using the vital dye trypan blue (0.4%). The remaining pieces were divided into 2 groups: Group 1 was exposed for 25 minutes to equilibration solution comprising of 7.5 % dimethyl sulfoxide (DMSO) and 7.5 % ethylene glycol (EG) followed by vitrification solution (20 % DMSO, 20 % ethylene glycol and 0.4M sucrose) for 15 minutes and immediately immersed in liquid nitrogen. Group 2 was exposed to the same equilibration solution for 10 minutes followed by vitrification solution (15 % DMSO, 15 % ethylene glycol and 0.4M sucrose) for 2 minutes and immersed in liquid nitrogen. Warming in Group 1 was done on sucrose 1M and 0.5M for 1 and 5 minutes respectively, followed by 10 minutes in HTF - Modified (Irvine®). Warming in Group 2 was performed in 1M sucrose, 0.5M and 0.25M for 5 minutes each. Follicular cells viability was analyzed after warming.
Results: Rates of follicle cell viability were 81.31 % and 90.81 % for groups 1 and 2 respectively.
Conclusions: The two ovarian tissue vitrification protocol in prepubertal female rats showed satisfactory results with potential for use for cryopreservation and transplantation.
P-32. Vitrification of immature testicular tissue in wistar rats
Larissa Benvenutti1, Leticia Wietcovsky1, Eduardo S A Velazquez1, Rafael A Salvador1, David Til1, Vera L L Amaral1
1UNIVALI - Universidade do Vale do Itajaí
Objective: Test the efficiency of two different protocols for immature testicular tissue vitrification.
Methods: After the orchiectomy, four testicles were divided into 3mm fragments for vitrification. The cell viability of fresh and vitrified fragments was accessed with Trypan Blue (0.4%) exclusion assay. The fragments were divided into Group 1 (n=6): vitrified with Ingámed® commercial vitrification kit, which were exposed to an equilibrium solution (VS1) for 10 minutes and posteriorly to a vitrification solution (VS2) for 5 minutes, and Group 2 (n=6) in which the fragments were exposed to an equilibrium solution composed of dimethyl sulfoxide 10% (DMSO), ethylene glycol 10% (EG) for 10 minutes, and posteriorly to a vitrification solution (DMSO 20%, EG 20% and 0.5M sucrose) for 5 minutes. Samples of both groups were placed in calibrated plastic innoculation loops (1ul) inside cryovials and immediately immersed into liquid nitrogen. Group 1 was thawed using Ingámed® thawing commercial kit. Samples were exposed to DV1 for 1 minute, followed by DV2 and DV3 for 5 minutes each one. Group 2 fragments were thawed using warming solutions in decreasing sucrose concentrations, 1M for 1 minute, 0.5M, 0.25M, and 0M for 5 minutes each one.
Results: Cell viability recovered rate was 81.31% ±5.2 for group 1 and 75.8±5.2 for group 2.
Conclusions: Both protocols showed positive results of viability cell recovery, exhibiting potential use for testicular tissue cryopreservation.
P-33. First pregnancy in Brazil resulting from criopreservated blastocyst obtained from in vitro matured oocytes
Priscila P C Scalco1, Marcos Hoher1, Nilo Frantz1, Marcos I R Kulmann1, Simone S Mattiello1, Gerta Frantz1, Norma P de Oliveira1, Caroline G Dutra1, Daiane M Paguiarin1
1Centro de Reprodução Humana Nilo Frantz, Porto Alegre/RS, Brazil
Introduction: In vitro maturation (IVM) is an option for infertile couples, especially for women with polycystic ovary syndrome (PCOS). Among the benefits of this technique are the ovarian hyperstimulation syndrome (OHSS) reduction, lower costs and method feasibility.
Case Report: A thirty six-year old PCOS patient whose partner was vasectomized 25 years ago, came to our clinic for IVF. The couple had already made two previous cryopreserved embryo transfers elsewhere. She became pregnant once but suffered a miscarriage. After immunologic investigation and considering her Anti-Müllerian Hormone (AMH) levels (16, 35 ng/mL), IVM was proposed to the couple. The oocyte retrieval was done after 36h of HCG injection. Cumulus-oocyte complex were cultured for 32 hours and after intracytoplasmatic sperm injection (ICSI), 10 matured oocytes fertilized. Fresh grade 2 (G2) embryos were transferred on day 3 (D3) of the same IVF cycle however implantation did not occur. The surplus embryos remained in culture and were vitrified on day 6 (D6). In the following cycle, the patient received oral estrogen and vaginal progesterone when both embryos were warmed and transferred. The dosage of β-HCG was 133 mIU/ml in the 10 day post-transfer. After 4 weeks, the ultrasonography showed an embryo heart beat.
Comments: IVM is a promising technique when applied to PCOS patients providing good quality blastocysts which, after proper vitrification, may be warmed and transferred resulting in a healthy pregnancy.
P-34. Oocyte and embryo quality in endometriosis
Kazue H Ribeiro1, Mila H R Cerqueira1, Gustavo C E Silva1, Vanessa N P Perez1, Rayssa A de Lima1
1CLINIFERT – Florianópolis/SC, Brazil
Objective: The aim of this study was to evaluate oocyte and embryo quality in patients with endometriosis versus patients with other factors, submitted to assisted reproduction cycles in CliniFert clinic.
Methods: We analyzed 203 cycles of IVF, oocytes 2025 and 1168 embryos. As a control group, were used cases of tubal factor, polycystic ovarian syndrome, low ovarian reserve, idiopathic infertility and male factor. The parameters for morphological analysis of oocytes and embryos were: maturation stage, color, granularity, resistance to ICSI, fertilization rate, symmetry of the blastomeres and percentage of fragmentation.
Results: Women with endometriosis showed 78.38% of mature oocytes, 46.06% with resistance to ICSI and 76.66% fertilized. 74.10% had alterations of zona pellucida, 69.35% dark ooplasm and 83.33% granular ooplasm. In 72 hours of development, 59.69% of embryos were asymmetric and 55.32% some level of fragmentation. In control group, 76.49% of aspirated oocytes were in mature stage, 44.26% had resistance to ICSI and 74.57% were fertilized. 65.83% had abnormalities in the zona pellucida, 73.50% dark ooplasm and 79.67% granular ooplasm. At 72 hours of development, embryos had 64.81% of bastomeres asymmetric and 63.17% with some level of fragmentation.
Conclusions: In this study, endometriosis no had effect on fertilization rate, but also has not been associated with a higher percentage of fragmentation and asymmetry of the blastomeres.
P-35. Does the blastocoele expansion degree interfere with blastocysts vitrification protocol?
Tamara Lamim1, Vera L L Amaral2, David Til2, Rafael A Salvador2, Marcel Frajblat3, Angélica Siewert1, Leticia Wietcovsky1
1Laboratório de Biotecnologia da Reprodução - LBR/UNIVALI, Itajaí/SC, Brazil
2Universidade do Vale do Itajaí – UNIVALI,Itajaí/SC, Brazil
3Universidade Federal do Rio de Janeiro – UFRJ/RJ, Brazil
Objective: Association between equilibration time and degree of expansion on blastocyst vitrification.
Methods: 36 female mice F1 (BALB/C X C57BL/6) were superovulated with eCG 10 IU (Equine chorionic gonadotropin - Novormon® - Synthex ) and , after 48 hours, with 10 IU of hCG ( Human Chorionic Gonadotropin - Vetecor® - Calier ).Three days after mating, the oviducts were collected and washed with medium GV- Hepes (Ingámed®) for recovery of embryos at morula stage. Embryos (n = 414) were cultured in GV -Blast (Ingámed®) supplemented with 10 % serum SI (Ingámed®) to blastocyst stage and divided into 3 groups: early blastocyst (B1) , blastocyst with 50 % blastocele expansion (B2) and expanded blastocyst (B3). Blastocysts were vitrified with kit Ingámed® and Vitri-Inga Ingámed® rods as the according to the manufacturer’s protocol. Different times for equilibrium solution (VI-1) were tested (15, 16, 17 and 18 minutes). Embryos warming followed Ingámed® protocol and evaluation of the hatching rate was performed after embryo culture.
Results: Hatching rates observed were to group B1 (94 %, 96 %, 85 % and 86 %), B2 (84 %, 91 %, 97 % and 97 %) and B3 (50 %, 64 %, 62% and 68 %) in time of 15, 16, 17 and 18 minutes, respectively.
Conclusions: Exposure times showed that best hatching rates for the groups B1 , B2 and B3 , were respectively 16, 18, 18 minutes, confirming the importance of equilibration time for blastocoele dehydration.
P-36. Prevalence of hysteroscopy alterations in women undergoing in vitro fertilization: cost-benefit analysis of screening hysteroscopy
Cecília de Souza Monteiro1
1Laboratório de Reprodução Humana do Hospital das Clínicas da Universidade Federal de Minas Gerais
Objective: Hysteroscopy as part of the basic workup for in vitro fertilization (IVF) has been subjected to extensive discussion by experts. The prevalence of abnormalities in hysteroscopy in women with normal clinical and image findings varies between 20% and 40%. The objective of this study was to evaluate the prevalence of uterine cavity abnormalities in pre-IVF screening hysteroscopies.
Methods: We included 135 consecutive women younger than 50 years old with normal transvaginal ultrasound and hysterosalpingography who underwent hysteroscopy in preparation for IVF during the year 2015 in an academic hospital of Belo Horizonte, Brazil. All hysteroscopies were performed in an outpatient setting without anesthesia using a hysteroscope with a 5 mm outer sheath. The sample size was calculated to estimate the prevalence of hysteroscopic alterations with 8% precision at 95% confidence level and 80% statistical power.
Results: Abnormal hysteroscopic findings were identified in 38 of 135 patients, yielding a prevalence of 28% (95% confidence interval 21%-36%). The prevalence of each alteration found in the screening hysteroscopy was: polyp (18%), adhesion (7%), endometrial thickening (5%), myoma (4%), cervical stenosis (2%), endometritis (2%), tubal obstruction (1%), uterine malformation (1%). The only adverse effect of the procedure was mild pelvic discomfort and no major complications were observed.
Conclusions: The prevalence of 28% means that 4 histeroscopies are needed to find one abnormality that justifies the cancellation or postponement of the IVF cycle. Therefore, the potential benefit of incorporating routine hysteroscopy as a screening method before IVF seems to outweigh harm, due to the low complication rates of the procedure.
P-37. DNA fragmentation index can be reduced by dietary changes and antioxidant therapy increasing the euploidia rate in embryos undergoing preimplantation genetic screening: a case report
Marcos I R Kulmann1, Rosa L Silvestrim1, Norma P de Oliveira1, Carla G Basso1, Gerta N Frantz1, Caroline G Dutra1, Nilo Frantz1
1Centro de Reprodução Humana Nilo Frantz, Porto Alegre/RS, Brazil
Introduction: The sperm genetics seems to be an important issue to embryo ploidy state and IVF outcomes.
Case Report: She, 38 years old, BMI=20, had one ectopic pregnancy, suffered salpingectomy and right oophorectomy. He, 30 years old, BMI=26.1, has no history of male factor. They passed through five IVF previous cycles elsewhere, four did not result in pregnancy and the fifth had no transfer because all biopsied embryos were aneuploid. Before the next attempt, it was recommended the Sperm Cromathin Structure Assay (SCSA) that resulted in 47% of DNA Fragmentation Index (DFI). The patient was advised to incorporate into his diet foods with antioxidant and anti-inflammatory properties, decrease the consumption of coffee, alcohol and gluten and refrain from using materials that could release xenobiotics. Daily supplementation of vitamin C (1g), vitamin E (600mg), chelated zinc (25mg), folic acid (5mg) and acetyl-L-carnitine (1g) were also prescribed. After three months, he repeated the SCSA resulting in 4% of DFI and a new IVF cycle was attempted. They got five MII oocytes and four of them fertilized. Five days later, two blastocists were biopsied, vitrified and both diagnosed as euploid. In a new cycle, one of the embryos was warmed up and transferred. Beta-HCG was positive and clinical pregnancy was confirmed with one gestational sac and heartbeat.
Comments: The report shows that bad initial sperm DFI can be easily reverted and result in successful IVF outcomes by a simple change of lifestyle, improvement of dietary habits and adequate use of antioxidants.
P-38. Endometriosis affects blastulation in art?
Emily de Conto1,2, Juliana G Silveira1, Vanessa K Genro2, Rita de Cassia B Chapon1,2, Daniela S da Silva2, Joao S da Cunha-Filho1,2
1UFRGS - Universidade Federal do Rio Grande do Sul, Porto Alegre/RS, Brazil
2Insemine - Centro de Reprodução Humana, Porto Alegre, RS, Brazil
Objective: Comparison of blastulation in patients undergoing in vitro fertilization with endometriosis and tubal factor.
Methods: This is a prospective study that recruited 76 women undergoing in vitro fertilization. Those patients were divided into two groups according to the cause of infertility: the first group had 44 patients with endometriosis and the other group had 32 patients with tubal factor.
Results: Primary outcome was blastulation, showing a mean rate of 46.13% for the endometriosis group and 48.10% for the tubal factor group (P = 0.966). The mean age of the patients showed no statistical difference between groups (P = 0.108) as well as Antral Follicle Count (P = 0.216), serum FSH levels (P = 0.143) and AMH (P = 0.419), initial dose gonadotropin (P = 0.083), number of oocytes retrieved (P = 0994), number of embryos generated (P = 0.880) and mean embryo score (P = 0.886). The statistical test used was the Student’s t test and we used the statistical program IBM SPSS Statistics 20. P value ≤ 0.05 was considered statistically significant.
Conclusions: There is no difference in blastulation rate between the studied groups. This outcome demonstrate that endometriosis do not cause damage in assisted reproductive technology cycles regarding the chance of blastocyst generation when compared to tubal factor.
P-39. Case report of zika virus during the controlled ovarian hyperstimulation: results from follicular fluid and cumulus cells
Edilberto Araujo Filho1, Cássio L Fácio1, Ligiane A M de Paula1, Ciro D Martinhago2, Ligia F Previato1
1Centro de Reprodução Humana de São José do Rio Preto (CRH-Rio Preto), São José do Rio Preto/ SP, Brazil
2Chromosome Medicina Genômica, São Paulo/ SP, Brazil
Introduction: Zika virus (ZIKV) is transmitted by Aedes aegypti, first report in Brazil in 2015.
Case Report: A 37-year-old female, indicated for in vitro fertilization (IVF) due to bilateral tubal factor, initiated ovulation induction on day 2 of the menstrual cycle. One day later, she traveled with her mother and sister, taking the medications. She returned and came to ultrasound on day 5 of the medication, showing skin rash on the trunk and legs, spreading to limbs. She reported that her mother and sister began same symptoms. Patient had 37°C, mild low back pain and joint pain no significant. Complete blood count (CBC) did not show platelets and leukocytes alterations. It was drawn blood of the patient and husband to test ZIKV by PCR. She offered to follow treatment until oocyte aspiration, as far as the clinic took care of the spendings. Oocyte aspiration was made 36 hours after hCG administration. It was retrieved 7 oocytes, follicular fluid, granulosa cells, and semen of the husband, all donated for study. PCR results for ZIKV in the blood was positive for her, and negative for husband, showing that he was not infected sexually. Analysis of follicular fluid and cumulus cells was performed using RT-PCR in real time and results were negative for both materials, which RNA of the ZIKV was not detected.
Comments: Absence of ZIKV in the follicular fluid and cumulus cells is the first report in the literature and that helped the better understanding of transmission and infection of this virus.
P-40. Oocyte per antral follicle count recuperation rate by using GnRH agonist to trigger follicle maturation in oocyte donation cycles
Ana P Aquino1, Tatiana C S Bonetti1, Eduardo L A da Motta1, Paulo C Serafini1, Talita G S Devecchi1, Carolina Kimati1, Bruna Barros1, Thais S Domingues1
1Huntington Medicina Reprodutiva, Sao Paulo/SP, Brazil
Objective: Controlled ovarian stimulation (COS) aim to recover as much oocytes as the ovarian reserve limit. The antral follicles count (AFC) is used as a predictor of the number of mature oocytes (MII), and it is estimated that MII oocytes recovered is at a 1 to 1 ratio to the AFC. The aim of this study was to evaluate the recovery rate of MII/CFA when using hCG or GnRH agonist to trigger in oocyte donation cycles.
Methods: This retrospective cohort study included 512 oocyte donation cycles carried out in 2013-2015. Patients were 18 to 35 years and AFC ≥10. The ovarian stimulation was obtained by using urinary or recombinant FSH and the trigger was given with hCG (Ovidrel, Merck Serono; n=36) or GnRH agonist (Gonapeptyl, Ferring; n=476). The MII/AFC ratio was calculated and compared between groups.
Results: The number of MII recovered was higher in the GnRH group (19.0) than hCG (10.9, P<0.001). MII/AFC ratio was 71.8% for hCG and 99.1% for GnRH groups (P<0.001). To evaluate the association of GnRH agonist trigger in the MII/AFC ratio, we carried out a multiple linear regression. The use of GnRH agonist trigger positively influenced the MII/CFA ratio (Coef. 28.5; P<0.001), adjusted to women age, FSH dose and body mass index.
Conclusions: GnRH agonist trigger prompt a MII/CFA ratio close to 100%, while hCG result in a 30% less MII/CFA ratio than estimated. The higher performance of GnRH agonist trigger, associated to prevention of ovarian hyperstimulation syndrome suggest it should be broadly indicated.
P-41. Learning about blastocyst culture from a pre-implantation genetic screening (PGS) program
Maria C Cardoso1, Alessandra Evangelista1, Juliana F. Cuzzi2, Cássio A Sartório1, Vivian Sant’anna1, Caio L V Werneck1, Ana P S Aguiar1, Paulo G de Sá1, Maria C E C Martins1
1Vida Centro de Fertilidade, Rio de Janeiro/RJ, Brazil
2Genesis Genetics Brazil
Objetive: The aim of this study is to verify if the time of blastocyst development and morphological parameters influence euploidy or aneuploidy or its implant capacity when it reaches the ideal moment for biopsy.
Methods: There were 206 cycles from 157 women (average age 38,9 years-old ranging from 24 to 46 years old) with at least one embryo for biopsy for PGS, during the years 2014 and 2015. 557 embryos developed to blastocyst stage and had their development time and morphological classification written down at the biopsy moment. The eggs with 0PN, 1PN and 2PN were cultivated until day 4 for assisted hatching (AH). From day 5 morning on, the embryos were periodically evaluated to look for the extrusion presence of trophectoderm through the hole made by AH in the zona pellucida - the biopsy moment. The morphological classification was appointed at the moment of the biopsy. The embryos with development block or that presented degeneration signals in their cells were discarded.
Results: Biopsies occurred within a minimum of 96 hours of development following ICSI and a maximum of 169 hours. From the 557 blastocysts analyzed, 24 (4.3%) had no DNA or degraded DNA for analysis and 158 (28.4%) were euploid. Among the aneuploidies, 106 (19.0%) were complex, 23 (4.19%) multiple, 77 (13.8%) dual, 59 (10.6%) single monossomy, 57 (10.3%) single trisomy and 53 (9.51%) part gain or part loss. There were no differences between euploid and aneuploidy embryos in relation to the blastocyst degree of expansion (P=0,99) and for IMC (P=0,95) and trophectoderm morphology (P=0,85), however, there was no implantation from euploid embryo with grade C for IMC or trophectoderm morphology. The average time of evolution for biopsy of euploid embryos was 124h (± 13,1h) and aneuploidy was 126h (± 14,4h) (P = 0.11). From the 158 euploid embryos, 97 were transferred (61 remain frozen) and 39 (40.2%) implanted. The average time of evolution for biopsy of embryos which were implanted was 121h (± 12,3h) and those who have not been implanted was 125h (± 11,3h) (P = 0.12).
Conclusions: The ideal time for embryo biopsy did not have any association with the embryo’s morphological quality either with euploidy or aneuploidy. Each embryo has its own time of development, regardless been euploidy or aneuploidy, morphological classification or implantation capacity. Results indicate that a single embryo transfer program can benefit of freezing all the embryos during blastocyst phase. The blastocysts with better morphological classification can be selected later for a transfer.
P-42. Two successful births using in vitro maturation (IVM) technique in same patient within a period of seven years
Caroline G Dutra1, Simone S Mattiello1, Gerta N Frantz1, Norma P de Oliveira1, Carla G Basso1, Marcos I R Kulmann1, Marcos Hoher1, Nilo Frantz1
1Centro de Reprodução Humana Nilo Frantz - Porto Alegre/RS, Brazil
Introduction: In vitro maturation (IVM) technique is an effective alternative for patients with polycystic ovary (PCO) because there is no need of exogenous gonadotropins avoiding completely the risks of ovarian hyperstimulation syndrome (OHSS).
Case Report: NEP, 23 years old in 2008, with PCO diagnosis, applied to our IVM program and, after 38 weeks of gestation, a healthy baby girl was born. In 2015, she returned for a second IVM trial. The natural cycle was controlled through ultrasound and 36 hours before the follicular pick up. 10.000UI of hCG (Choriomon®) was administered. Five cumullus-oophorus complex (COCs), were collected using a 19 Gauge needle (Cook) and 75-80 mmHg pressure, guided with transvaginal ultrasound (Ultrasonix Op, Sonix). The COCs were cultured on preincubation media (LAG – MediCult®) for 3 hours and then transferred to maturation media (IVM – MediCult®) supplemented with 75 UI FSH and 75 UI hCG , for 32 hours. Four matured oocytes were fertilized with ICSI, resulting in four embryos. Three embryos were transferred as follows: 2 grade 2 and 1 grade 3, using a Wallace Sure-ProTM catheter. After 10 days the B-hCG exam was positive and the gestation went forward until 39 weeks. A healthy baby was born by cesarean, weighing 3,575 kg and 49 cm.
Comments: PCO patients can benefit from IVM avoiding completely the risks of OHS. The correct application of IVM can offer costs and management advantages and is highly recommended for patients that cannot be hormonally stimulated.
P-43. The effect of body mass index on the assisted reproductive outcomes for polycystic ovary patients
Marcos I R Kulmann1, Carla G Basso1, Norma P de Oliveira1, Gerta N Frantz1, Caroline G Dutra1, Joana C Chagas1, Fernanda Robin1, Nilo Frantz1
1Centro de Reprodução Humana Nilo Frantz, Porto Alegre/ RS, Brazil
Objective: Verify how BMI can affect pregnancy rates of PCO/PCOS women after fresh or frozen embryo transfers .
Methods: This is a retrospective study from 65 PCO/PCOS patients that underwent IVF-ICSI from 2012 to 2016. Patients were split according to BMI (>25 or <25) and to fresh or frozen embryo transfer (ET). Four groups were formed : Fresh+BMI>25 (n=16), Fresh+BMI<25 (n=26), Frozen+BMI>25 (n=6) and Frozen+BMI<25 (n=17). PGD cycles and those involving severe male factor were not included. We compared cycle variables and rates between groups with the same kind of ET. We used Student’s t test and Fisher’s exact test to analyze the results, considering P<0.05 as statistically different.
Results: Comparisons were not significant according to age, days of medication, endometrium , number of mature oocytes, fertilization rate and embryos transferred. Concerning fresh ET, we observed a decreased number of follicles (P=0.0479) and oocytes (P=0.0449) comparing the BMI>25 group (BMI=31.4±4.8) to the BMI<25 group (BMI=21.1±1.9). In these fresh ET, clinical pregnancy rate was 50% and 61.53%, respectively (P=0.5314). Concerning frozen ET, we observed a decreased number of follicles (P=0.0391) comparing the BMI>25 group (BMI=30.5±3.7) to the BMI<25 group (BMI=21.2±2.3). In these frozen ET, clinical pregnancy rate was 33,3% and 58,8%, respectively (P=0.3707).
Conclusions: Since obesity appears in more than one half of PCO/PCOS women, BMI effect may be relevant when studying IVF outcomes. We found out a trend of better clinical pregnancy in patients with appropriate BMI, though not statistically significant. We believe that further studies may clear up these issues.
P-44. A molecular biology laboratory experience with preimplantation genetic screening (PGS) by the next generation sequencing (NGS)
Vinicius B da Rosa1, Ana P Peixoto1, José A Lucca Neto1, Alessandro Schuffner1
1Clínica Conceber - Centro de Medicina Reprodutiva, Curitiba/PR, Brazil
Objective: To report the data obtained from embryos analyzed by NGS technique for detection of chromosomal aneuploidy.
Methods: It was analyzed using next generation sequencing (NGS) the DNA of 49 blastocysts from 18 patients aged 31 to 43 years, from December 2015 to May 2016. The sequencing was performed on the Ion Torrent - Personal Genome Machine® (Life Technologies), with semiconductor technology. The samples were sequencing using 314v2 and 316v2 chips allowing an average of 150.000 reads per sample (embryo). The analysis of the sequencing was performed using the low-pass whole-genome protocol by Copy number variation (CNV) using the ion Reporter v.5.0 software.
Results: Of the 49 embryos analyzed, 29 were diagnosed as euploid (59.2%), 19 diagnosed as aneuploid (38.8%) and 01 showed amplification failure (2%).
Conclusions: The results obtained by the molecular biology laboratory for embryonic euploidys are according to data published internationally. Based on these results we can conclude that the methodology provides consistent results, offering to the patients a safe tool for genetic analysis.
P-45. Freeze-all embryos policy in IVF/ICSI cycles. Chance of pregnancy after vitrified and thawed embryo transfer in a closed system, using Lupron® or Ovidrel® during the final maturation
Rodopiano S Florencio1, Lidia R Z O Castro1, Jane P Rocha1, Mariana P Batista1, Vinicius A de Oliveira1, Eduardo C Castro1, Mylena N C Rocha1
1Humana Medicina Reprodutiva Goiânia/ GO, Brazil
Objective: To determine the chance of pregnancy in patients subjected to IVF/ICSI procedures, up to 39 years of age, who underwent transfer of vitrified/thawed embryos in a closed system, Irvine®.
Methods: One hundred ninety six patients normo/hyperresponder underwent IVF/ICSI procedures between 2014 and 2015. 33 patients included in the presente study, with 39 years old or less, had all embryos frozen/thawed within that period, by the vitrification method in a closed system (Irvine®) regardless of the indication for the procedure. All patients with indication for IVF/ICSI after the clinical investigation were submitted to ovulation induction with gonadotropin recombinant or not, associated with LH or not, at a daily dose of 150 to 300 IU sc. from the 2nd day of the cycle. Patients received Ovidrel® 250 or Lupron Kit 0.4 ml sc for the final follicular maturation. The ovum pick-up was performed 35-36 hours after maturation, by manual aspiration and rarely through a suction pump. There was no fresh embryos transfer. In most cases, we considered the freezing of all embryos, due to the risk of ovarian hyperstimulation syndrome (OHSS). The group of patients using Lupron kit® had large percentage of fresh embryo transfer(41,5% of pregnancy) and a small percentage of freeze-all embryo transfer. The endometrial preparation for thawed embryo transfer was performed using oral Primogyna® 2mg 8/8 h and/or Estradot® 100, 1 daily patch. The remaining patients underwent a natural cycle embryo transfer. The patients were treated with vaginal Utrogestan® 200mg 8/8 h when the endometrium reached a satisfactory extent and embryo transfer was carried out after 5 or 6 days after taking the medicine. The embryo transfer procedure was performed using Sidney® transfer catheter. We evaluated the chance of pregnancy per transfer and per patient in two groups of final maturation.
Results: Thirty three patients had all embryos frozen by vitrification and thawed during the period of the study,with 47 transfer. The total number of frozen embryos in the period was 234 (average of 7.1/patient), 116 from which were thawed and 102 (87.9%) survived. The average embryo transfer per patient in the period was 1.42. The chance of pregnancy/transfer in freeze group was 42,5%. The group using Lupron® (group 1), underwent 8 transfers in 6 patients and showed 5/8 (62.5% of pregnancy). The Ovidrel® group (group 2), underwent 39 embryo transfer in 27 patients, resulting in 15/39 (38.4%) of pregnancy. For the first group, 87.5% of embryo transfer occurred with 1 or more blastocysts and for the second group this rate was 66.6%. The rate of pregnancy / patient in the first group was 83.3% and 40.7% in the second.
Conclusions: Our results for freeze-all embryos policy in two years, showed a trend toward large percentage of fresh embryo transfer when Lupron® is used in order to prevent OHSS and few cases of this group for freezing/thawing procedures. This data showed similar results (42,5%/41,5%) of freeze all and fresh transfer in our clinic.
P-46. Oocyte in vitro maturation technique in an oncofertility perspective
Juliana A Lopes1, Bruna T G M Jianini1, Jhenifer K Rodrigues1,2,3
1Associação Instituto Sapientiae, São Paulo/SP, Brazil
2In Vitro Consultoria, Belo Horizonte/MG, Brazil
3Latin America Global Oncofertility Network Oncofertility Consortium
Objective: Technique of oocyte in vitro maturation (IVM) was first demonstrated by Pincus and Enzmann in 1935 using rabbit oocytes. It consists in the retrieving of immature oocytes from unstimulated or minimally stimulated follicles (< 10 mm), which are arrested in the prophase of first meiotic division, and its maturation to metaphase II. The technique of IVM allows to culture cumulus oophorus complexes (COC) from small- and medium-sized (2 to 10 mm) follicles, and freeze the mature oocytes. The technique is effective for oncological patients, including prepuberbal girls. Another possibility is the retrieval of immature oocytes ex vivo at the time of ovary processing before its cryopreservation, and its maturation in vitro followed by vitrification. Our objective was to discuss the role of IVM technique in the strategy of fertility preservation and recent research results and questions that are still emerging on the topic.
Methods: Review of the literature through a survey using online databases as Latin American and Caribbean Health Sciences (Lilacs), Pubmed and Cochrane Library through keywords.
Results: It was found that IVM now has been used in a few laboratories around the world, and has been shown excellent results. About three thousand live births has been already reported. However, it requires further optimization.
Conclusions: IVM is a promising technique, despite the technical challenges. And it has been considered a great alternative for preservation of gametes in female cancer patients, especially for prepubertal girls and for those who have urgency in starting the anti-neoplastic treatment.
P-47. Positive outcome of chance in ar cycles per season
Emily de Conto1,2, Renata Bohn1, Marco Vinicius A S B Fleuri1, Vanessa K Genro2, Rita de Cassia B Chapon1,2, Daniela S da Silva2, Joao S da Cunha-Filho1,2
1UFRGS - Universidade Federal do Rio Grande do Sul, Porto Alegre/RS, Brazil
2Insemine - Centro de Reprodução Humana, Porto Alegre/RS, Brazil
Objective: To evaluate the reproductive outcome (positive βhCG) of assisted reproduction cycles (IVF-ICSI) according to the seasons in which they were made.
Methods: A prospective study evaluating 461 cycles of IVF in a center of human reproduction Porto Alegre / Brazil. These cycles were divided into 4 groups according to the season in which they were carried out: summer (n = 140), autumn (n = 124), winter (n = 99) and spring (n = 98). The statistical test was conducted test Chi Square for categorical variables and One-Way ANOVA for continuous variables. The statistical program used was SPSS Statistics 20 and P≤0.05 value was considered statistically significant.
Results: The mean age of patients was 35.05±2.9 no statistical significance (P = 0.136), the serum level FSH was 7.9±3.7 IU/L (P = 0.464) and the initial dose of gonadotropin 255.8±65.6 (P = 1.000). Laboratory data cycles also showed no significant difference, and the mean number of oocytes retrieved was 27.5±4.4 (P = 0.901), MII oocytes 4.72±3.7 (P = 0637), fertilized oocytes 3.0±2.7 (P = 0.589), embryos generated 24.3±2.9 (P = 0682) and mean embryo score 61.6±25.1 (P = 0.846). The frequency of positive results for the season was 31.4% for the summer, 23.4% for the fall, 22.2% for winter and 32.6% for spring, with P = 0.186.
Conclusions: Our results indicate that there is no correlation between the seasons and the positive or negative result of pregnancy in RA cycles.
P-48. IVF/ICSI Endometrial thick-
ness on the day of final follicular maturation and chance of pregnancy in hyperstimulated cycles
Jane P Rocha1, Marta C C F Finotti1, Mariana P Batista1, Mirian R Borges1, Vinicius A de Oliveira1, Eduardo C Castro1, Rodopiano S Florencio1
1Humana Medicina Reprodutiva Goiânia/GO, Brazil
Objective: To determine the chance of pregnancy in patients subjected to IVF/ICSI procedures, 39 years old or younger, who underwent fresh embryo transfer (type 1, 2 or 3) in three groups of endometrial thickness: <7mm, 7-9mm and ≥10mm.
Methods: Our study group comprises 711 patients undergoing ICSI, from 2010-15, with 39 years old or younger. The fresh embryo transfer was carried out in patients undergoing IVF/ICSI through types 1, 2 and 3, regardless of the indication for the procedure. Embryos showed suitable cleavage stage in the day of transfer (2 embryos were type 1, 1 embryo was type 2 and type 3 for embryos with 24 hours delayed or arrested cleavage). Donors and recipients were excluded. All patients with indication for IVF/ICSI after the clinical investigation were submitted to ovulation induction with gonadotropin recombinant or not, associated with LH or not, at a daily dose of 150 to 300 IU sc. from the 2nd day of the cycle. The microdose GnRH agonist was used as an adjunct to gonadotropin therapy in a long-acting GnRH regimen, associated to birth control pill in the previous cycle or with GnRH antagonists for patients with dominant follicles 13-14mm. Patients received Ovidrel® 250 or Lupron Kit 0.4 ml sc for the final follicular maturation. Luteal phase maintenance was performed with oral or patch estrogen, vaginal or intramuscular progesterone or low Ovidrel® doses, depending on the drug used for the final follicular maturation. We assessed the chance of pregnancy in 3 groups of patients, according to the endometrial thickness measure: <7mm (A), n=15; 7-9mm (B), n=256; and ≥10mm (C), n=440 in the day of the final follicular maturation. We also evaluated the average age, the day of embryo transfer, average of transferred embryos. Statistical tests were considered significant for P <0.05. Results: The study groups showed no significant statistical difference for the variables that were analyzed; average age (33.8/32.9/33.6 p(B/C)=0.3500), average number of transferred embryos (2.4/2.3/2.3 p(B/C)=0.1404) and transfer day average (3.9/3.8/3.9 p(B/C)=0.2014). The chance of pregnancy in the groups was: A (3/15, 20%), B (103/156, 40.2%), C (185/440, 42.0%). The chi-square showed the evaluation for the groups, 0.2044, and a/b=0.1185, b/c=0.6399 and a/c=0.0881.
Conclusions: Our results presented through this study show that the endometrial thickness measured on the day of final maturation had no significant differences among the groups. The small number of cases in group A may have influenced these results. Thus, the selection criteria for the study was not an important prognostic variable for pregnancy, especially if we consider only the patients with endometrial thickness equal or higher than 7mm.
P-49. Murine oocyte in vitro maturation, with and without ovarian stimulation, in different commercial media of embryo culture
Eduardo S A Velazquez1, David Til1, Rafael A Salvador1, Marcel Frajblat2, Vera L L Amaral1
1Universidade do Vale do Itajai-UNIVALI, Itajai/ SC, Brazil
2Universidade Federal do Rio de Janeiro –UFRJ/ RJ, Brazil
Objective: The present study compared the efficiency of commercial culture media on oocyte maturation, with and without ovarian stimulation.
Methods: F1 female mice (Balb/C x C57Bl/6) were randomly divided in: group A, with ovarian stimulation (10 IU eCG, Novormon®); and group B without stimulation. The ovaries were dissected in GV-Hepes medium (Ingámed®) and oocytes (n=496) presenting germinal vesicle were selected and divided for maturation in six different media: 1) G-1 TM Plus® (Vitrolife®); 2) G-2 TM Plus® (Vitrolife®); 3)GV Blast® (Ingámed®) + SSS (10%); 4) Sydney IVF Fertilization® (Cook Medical®); 5) Sydney IVF Blastocyst® (Cook Medical®); 6) Sydney IVF Cleavage® (Cook Medical®), incubated at 37°C under 5% CO2 for 24 hours.
Results: In vitro maturation was evaluated and metaphase II oocyte stage in groups A and B were respectively: 76% and 70.73% for G-1 TM Plus® (Vitrolife®); 65% and 64.86 for G-2 TM Plus® (Vitrolife®); 46% and 57.89% for GV Blast® (Ingámed®) + SSS (10%); 68.75% and 55.56% for Sydney IVF Fertilization® (Cook Medical®); 65.85% and 55.56% for Sydney IVF Blastocyst® (Cook Medical®); 68.18% and 45.71% for Sydney IVF Cleavage® (Cook Medical®).
Conclusions: G- 1 TM Plus® medium (Vitrolife®) showed subtly better response for oocytes from stimulated females, followed by the three Cook Medical® media. G-2 TM Plus® medium (Vitrolife®) presented similar results in both situations, whereas GV Blast® medium (Ingámed®) shows a bigger maturation potential for oocytes without stimulation, demonstrating that it is possible achieving reasonable in vitro maturation rates in commercial media of embryo culture.
P-50. The nursing consultation in Assisted Human Reproduction
Janaina F Aderaldo1, Nanete C da Costa Prado2, Dayane J C de Menezes2, Kleber M Morais1,2, Edualeide J P B da Nóbrega2, Mychelle M G Torres2, Kelley R N Barbosa1
1Empresa Brasileira de Serviços Hospitalares – EBSERH, Brazil
2Universidade Federal do Rio Grande do Norte – UFRN/RN, Brazil
Objective: The nurse perfomance as educator promotes a bond between the medical staff and the infertile couple. It is necessary that the nurse acting in Assisted Human Reproduction is qualified to performr these activities, thus contributing to an adequate assistance and aggrandizement of the profession. This paper aims at describing the nursing consultation in Assisted Human Reproduction.
Methods: It is an experience report in the Human Reproduction Center (HRC) in a renowed maternity hospital in the Northeast of Brazil.
Results: The nursing consultation is carried out in an individualized way, holisticaly evaluating the couple. The collected data in the anamnesis performed by the physician, as personal and family history, medication used, previous surgeries and the couple’s habits, help to choose the most appropriate treatment. After choosing the suitable treatment, the nurse gives orientation about the procedure’s stages, performs counseling to the signature of the consent form, clarifies the procedure to be performed and gives information about its duration; reinforces the importance of treatment assiduity and the correct administration of medication and its potential side effects and informs about the exams done during the treatment as well as about scheduling of appointments.
Conclusions: The nurse has a key role in the clarification of questions, in the lab exams evaluation and promotes emotional support to the couple, preparing them to the possibility of failure in the treatment and contributes to the couple’s compliance to the treatment and avoids inappropriate conducts that may interfer in the success of the treatment.
P-51. Xanthan gum as a cryoprotectant additive in human sperm preservation
Sabrina M R J Costa1,2, Fernanda G Valverde1, Conrado M Souza Neto1, Erika C Silveira2, George H C Silveira2, Francine F Padilha1, Isabel B L Verde1
1UNIT - Universidade Tiradentes, Aracaju/ SE, Brazil
2CEMISE - Centro de Medicina Integrada de Sergipe, Aracaju/ SE, Brazil
Objective: This study aimed to develop a cryoprotectant containing xanthan gum (XG) for human semen preservation.
Methods: It was used semen samples of patients who underwent spermogram in an assisted reproduction clinic (Aracaju/SE) and who met the inclusion criteria. Samples were divided into five groups: a)controls: (i)TYB (commercially available) and (ii)GEYC (Glycerol-Egg-Yolk-Citrate): prepared according to the WHO manual for human sêmen (2010); b)treaments: (iii)GEYC+0.15%XG; (iv)GEYC+0.20%XG; (v)GEYC+0.25%XG. Groups containing GEYC used WHO (2010) freezing protocol and TYB group freezing protocol was in accordance with product instructions. Sample thawing was performed at least 48h post-freezing. Parameters analyzed pre and post-freezing were: motility, concentration, vitality, morphology, plasma membranes integrity (PMI), acrosomal membrane integrity (AMI) and mitochondrial activity (MA).
Results: All cryopreserved groups decreased parameters when compared to fresh samples, but showed no difference between them. For motility, only XG0.20 showed no difference from GEYC. For vitality, only XG0.25 was different from TYB. Regarding morphology, all cryopreserved groups were similar. XG use as a cryoprotectant additive showed no harmful effects to PMI, AMI and MA at 0.15% and 0.20% concentrations. Only 0.25% concentration showed difference to TYB group considering sperm viability (normal PMI-AMI and high MA). Therefore, the lowest XG concentrations are shown to be a possible cryoprotective additive for human sperm.
Conclusions: Whereas in many parameters, treatments containing 0.15% and 0.20% XG concentration had similar results to control groups, this biopolymer addition in cryopreservation media in these concentrations showed that this biopolymer has great potential to be used as an additive in human semen cryoprotectant freeze media.
P-52. Clomiphene Citrate to prevent follicular rupture in oocytes and embryos vitrification cycles
Vinicius M Lopes1, Jean P B Brasileiro1, Joaquim R C Lopes2, Natalia I Z Tierno1, Thaisa S Lacerda1
1Instituto Verhum, Brasilia/DF, Brazil
2CENAFERT - Centro de Medicina Reprodutiva, Salvador/BA, Brazil
Objective: To evaluate the effectiveness of clomiphene citrate (CC) associated with ibuprofen to prevent follicular rupture in cycles of freezing oocytes and embryos.
Methods: All cases of ovarian stimulation for oocytes and embryos vitrification without GnRH antagonist for pituitary suppression between September 2015 and June 2016 were included. For ovarian stimulation were used 150 or 200 mg/CC/day during 5 days, beginning in the second or third day of the cycle. On day six of CC, the dose was reduced to 100 mg/day until one day after the trigger, performed with 10.000UI of hCG in the presence of two or more follicles over 18mm. Additionally was administered 600mg of ibuprofen orally in the night of the trigger and repeated 24 hours later. Oocyte pick-up was conducted between 35-36 hours after the trigger. Transvaginal ultrasound was performed before oocyte pick-up (OPU) to check the absence of follicular rupture.
Results: In 19 cycles were used only CC and in 15 cycles, it were associated with gonadotropins to perform the controlled ovarian stimulation. Thirty-four retrievals in 24 women were scheduled; only one case had follicular rupture before the procedure. The average of dominant follicles and mature oocytes (MII) obtained was 4.26 (± 1.88) and 4.24 (± 2.04) respectively.
Conclusions: The use of CC and ibuprofen was effective in preventing folicular rupture in all but one cycle. It is a possible option to avoid costs with GnRH antagonista when perform oocyte and embryo vitrification cycle.
P-53. Genetic polymorphisms association with poor responder in patients undergoing in vitro fertilization
Arivaldo Meireles1, Joao S da Cunha-Filho2, Pablo Sales1, Izabel Magalhaes3, Fabio Nascimento1, Panila L Lorenzzoni1, Jordana Castro3, Thiago B Gama3, João Paolo Bilibio1,3
1Clínica PRONATUS - Medicina Reprodutiva, Belém/ PA, Brazil
2UFRGS - Universidade Federal do Rio Grande do Sul, Porto Alegre/ RS, Brazil
3UFPA - Universidade Federal do Pará, Brazil
Objective: Approximately 10% of women seeking fertility treatment have diminished ovarian reserve (DOR). Gene association studies have identified a number of Single Nucleotide Polymorphisms (SNP) involved in the ovarian response. To evaluate the association of the major hormones and their receptors gene polymorphisms that were related to follicular development (FSH, LH, BMP-15, GDF9, and HAM) between poor and norm responders patients undergoing stimulation for IVF .
Methods: A Case control Study was performed. The included patients were norm responders and poor responders undergoing IVF. We performed DNA extraction of peripheral blood, followed by polymerase chain reaction to polymorphisms at FSH, LH, BMP-15, GDF9, and HAM and we valuate of presence of polymorphisms in patients poor and norm responder undergoing IVF.
Results: In the present study we showed that the presence of the c.398G> C polymorphism in the GDF9 gene is associated with poor response (PR) in infertile patients undergoing ovarian stimulation for IVF (68% in poor responder versus norm responders). Also the homozygous mutant genotype for the polymorphism c.447 C> T of the GDF9 gene was found in 50% and 19%, respectively in poor and normorespondedoras patients, evidencing the same way a strong association with poor ovarian response to ovulatória induction.
Conclusions: Thus we can conclude that GDF-9 398C> G polymorphism exerts an important influence on oocyte development. Besides of then, we need to perform functional studies to understand a real function e a possible correction and treatment to improve de number de oocytes retrieved in patients with GDF9 polymorphisms.
P-54. Fresh embryo transfer in IVF/ICSI cycles using Lupron® or Ovidrel® for final maturation and chance of pregnancy
Vinicius A de Oliveira1, Mirian R Borges1, Rodopiano S Florencio1, Jane P Rocha1, Mylena N C Rocha1, Corival L A de Castro1, Fernando C Santos1
1Humana Medicina Reprodutiva Goiânia/ GO, Brazil
Objective: To determine the chance of pregnancy in patients undergoing fresh embryo transfer in IVF/ICSI cycles with 6 or more ova collected, in an age group less than or equal to 39 years old, with Lupron® or Ovidrel® in order to reach final maturation.
Methods: Five hundred ninety eight patients normo and hyper responders, 39 years old or younger undergoing ICSI from 2010 to 2015, with at least 6 collected eggs regardless of the indicated procedure for the collection. All of the patients underwent fresh embryo transfer and all patients undergoing freeze-all embryo transfer were excluded from the study. All patients with indication for IVF/ICSI after the clinical investigation were submitted to ovulation induction with gonadotropin recombinant or not, associated with LH or not, at a daily dose of 150 to 300 IU sc. from the 2nd day of the cycle. The microdose GnRH agonist was used as an adjunct to gonadotropin therapy in a long-acting GnRH regimen, associated to birth control pill in the previous cycle or with GnRH antagonists for patients with dominant follicles 13-14mm. Patients received Ovidrel® 250 or Lupron Kit® 0.4 ml sc for the final follicular maturation. Luteal phase support was performed with oral or patch estrogen, vaginal or intramuscular progesterone or low Ovidrel® doses, depending on the drug used for the final follicular maturation. The experimental group (EG) (using Lupron®), consisted of 89 patients and the control group (GC) (using Ovidrel®) consisted of 509 patients. In each group, we assessed the average age, number of embryo transfer, day of embryo transfer and the percentage of pregnancy. Statistically significant difference was considered for P <0.05.
Results: The EG results were statistically different from the GC results regarding the following variables: average age (30.3/32.7), average of injected eggs (12.6/7.9), average of formed embryos (8.9/5.5), average of embryo day transfer (4.2/3.9). There was no statistical significant difference for the average of embryo transfer (2.3/2.3) and the likelihood of pregnancy (41.4%/40.7%,
P=0.9033).
Conclusions: Our results show number of embryo transfer were similar for the two groups. There was no significant difference in the likelihood of pregnancy, in the fresh embryo transfer, but there was important difference in age, injected eggs, number of embryos formed and more cases of late transfer. A proper preparation of the luteal phase with use of Lupron® and the possibility of freeze all, enabled the implementation of a protocol with the intention of eradicate OHSS development in our clinic.
P-55. Fertility preservation for men: review on recent developed techniques for cryopreservation of a small number of sperm cells
Josiane B Dutra1, Bruna T G M Jianini1, Jhenifer K Rodrigues1,2,3
1Associação Instituto Sapientiae, São Paulo/ SP, Brazil
2In Vitro Consultoria, Belo Horizonte/ MG, Brazil
3Latin America Global Oncofertility Network Oncofertility Consortium
Objective: Subfertility affects about 10% to 15% of couples trying to conceive. Diseases such as cancer and autoimmune diseases can affects fertility directly or after treatment. Assisted Reproductive Techniques (ART) has improved so that men and women find the opportunity to preserve their gametes and possibly having a child in the future. Discuss current issues related to semen cryopreservation techniques and recent advances on the methods for cryopreservation of few sperm cells, which can be applied for cancer patients and patients with low sperm quality.
Methods: Review of the literature database in Latin American and Caribbean Health Sciences (Lilacs), Medical Literature Analysis and Retrieval System Online (Medline), Pubmed and Cochrane Library through keywords.
Results: Cryopreservation of few spermatozoa is still a major challenge for male fertility preservation in men, but methods have been developed. The use of micro-straws has been reported showing better sperm motility and acrosomal integrity than traditional 0.25 ml and 0.5 ml straws, possibility related to the thinner and very small volume, causing a faster freezing rate of micro-straws. Hollow-core agarose capsules also has been tested to the cryopreservation of one single sperm cell, method in which it is used the conventional intracytoplasmic sperm injection (ICSI) to insert the spermatozoa into the capsule and then it is cryopreserved on polycarbonate or nylon mesh sheets using nitrogen vapor.
Conclusions: Considering the importance of male fertility preservation to ensure the reproductive rights of families, these studies are fundamental and should further enhance for the effectiveness of ART.
P-56. Pre-implantation genetic screening (PGS) and the influence of maternal age on the incidence of embryonic aneuploidy
Moísa L Pedrosa1, Bruna O Martins1, Luiza M S Aguiar1, Márcia M Carneiro1, Ana Márcia M Cota1, Márcia C F Ferreira1, Rívia M Lamaita1
1Reprodução Humana Mater Dei, Belo Horizonte/MG, Brazil
Objective: Embryonic aneuploidy is believed to be responsible for 70% of first trimester miscarriages and its prevalence increases with maternal aging, occurring in up to 85% of the blastocysts of women over 43 years old. PGS selects euploid embryos and can be achieved through embryo biopsies on day 3 (blastomeres at cleavage stage) or day 5 (trophectoderm at blastocyst stage). In this study, we aimed at reporting and evaluating our experience with PGS.
Methods: Data of 15 PGS procedures performed from in 10 different patients from February 2015 to May 2016 were analyzed. Two patients had their embryos biopsied on day 3 and all the others on day 5. All samples were analyzed by CGH-array.
Results: Maternal age was the indication in 85% of cases. Patients were 36-42 years old. Out of the 22 biopsied embryos of patients aged 36-40 years, only 5 were euploid (22%). Patients over 40 years old had a total of 17 embryos analyzed, with no euploid ones. In this series, only one transfer of euploid embryo was carried out but no pregnancy resulted, what makes it impossible to assess live birth rates after the use of this technology.
Conclusions: Our findings confirm the role of maternal age as the main determining factor in the occurrence of embryonic aneuploidy, and demonstrate the importance of pre-implantation genetic screening in this group of patients as a way to pursue the transfer of healthy embryos and the birth of healthy babies.
P-57. Germinal tissue cryopreservation: potential fertility preservation alternative for male and female cancer patients
Mariana A S Reis1, Jhenifer K Rodrigues1,2,3
1Associação Instituto Sapientiae, São Paulo/SP, Brazil
2In Vitro Consultoria, Belo Horizonte/MG, Brazil
3Latin America Global Oncofertility Network - Oncofertility Consortium
Objetive: It was estimated for 2016, more than 500.000 new cases of cancer in Brazil. Advances in cancer diagnosis and therapy have improved survival rates. However, the treatment can adversely impact reproductive function. Although the options available for Fertility Preservation (FP), endorsed by the American Society of Reproductive Medicine and recommended by the American Society of Clinical Oncology, are cryopreservation of semen, embryo and mature oocytes following in vitro fertilization. The cryopreservation of germinal tissue is currently a very promising technique, but still considered as experimental both for ovarian and testicular tissue. The purpose of this study was a review presenting the FP options for cancer patients and to discuss outlines about the experimental methods among women and men cancer patients.
Methods: The literature on tissue cryopreservation was searched using online databases. The scientific background, current developments and potential applications of these methods were reviewed.
Results: The recent case reports and reviews has shown that cryopreservation of germinal tissue is a very promising technique. They are still considered experimental, however it has been reported already 60 live births and 5 ongoing pregnancies after ovarian tissue cryopreservation and transplantation, and recent tests has been shown promising results in banking testicular tissue to generate spermatogenesis from spermatogonial stem cells.
Conclusions: Studies provided data on safety and efficacy of established techniques, excellent options for male/female patients to preserve fertility. And recent studies have shown excellent results on ovarian and testicular tissue, with big mammals and humans, what should be discussed with patients.
P-58. Age assessment, type of infertility, marital union time and patient stress symptoms of infertile women submitted to music therapy in a brazilian university center
Eliamar A B Fleury1,2, Mário S Approbato1, Reinaldo S A Sasaki1, Mônica C S Maia1, Marisa S Ramos1, Fabiana C Approbato1, Maíra R Magri3, Flávia N M de Oliveira4, Yanna A R de Lima1
1Human Reproduction Center - Department of Obstetrics and Gynecology Clinical Hospital - Goias Federal University – Brazil
2Musical School and Scenic Arts/Goiás Federal University
3Catholic University of Goiás – Brazil
4Health Secretariat of District Federal
Objective: To verify age, type of infertility, marital union time and symptoms of stress in infertile women undergoing to music therapy interventions.
Methods: A descriptive study of 14 infertile women attended at a university center, between 21 and 41 years, randomly selected. We used sociodemographic and clinical questionnaire and Symptoms Inventory of Lipp Stress (SILS). We analyzed the following variables: age, type of infertility, marital union time and symptoms of stress. Analyses were performed using SPSS 21 and multivariate analyzes SPAD 7.4. Multiple correspondence analysis found the correlation between the variables and individuals and Hierarchical Cluster Analysis of samples similarities. It was considered p value lower than 0.05.
Results: 57.1% of the patients were between 21-35 years; 78.6% primary infertility and 57.1% have 6-14 years of marital relationship. The Hierarchical Cluster Analysis showed grouping of 7 clusters symptoms: dizziness/floating sensation and frequent dizziness; hyperventilation, change in appetite and doubt about him/herself; to think/to talk about one subject, sudden urge to start new projects, cold hands and feet; sleep-related disorders; sexual disorders and ulcers.
Conclusions: The age group with the highest prevalence was 21-35 years, the primary type infertility and marital union time was 6-14. The evaluated patients demonstrated similarity, likely to sleep disorders in clusters 3, 5 and 6, suggesting the importance of this aspect in future studies with infertile patients.
P-59. The use of 1 (one) frozen donor semen straw in 2 (two) fertilization in vitro cycles
Beatriz M Silva1, Rosaly R Costa1, Victor E T de Sousa1, Yamara A Macedo1
1Centro de Ensino e Pesquisa em Reprodução Assistida do Hospital Materno Infantil de Brasília - CEPRA/HMIB
Objective: To evaluate the feasibility of using half-cryopreserved donor semen straw by IVF / ICSI cycle in relation to the viability of sperm.
Methods: There were 03 couples in treatment in SUS (public hospital) entitled to only two attempts of IVF / ICSI. A straw containing 0.5 ml of cryopreserved semen was removed from liquid nitrogen and, immediately, cut in half with scissors. One half was processed in a discontinuous gradient. The other half was stored again in liquid nitrogen and kept until the next fertilization.
Results: One couple achieved pregnancy using one of the straw halves, while the other half was kept frozen for future use; the other two couples had the two halves used. Although, there was significant reduction in the number of mobile spermatozoa from 5 million to 300,000 between the straw halves, the fertilization rate remained at 60%. There was embryo transfer in D3 and D5 with surplus embryo freezing in D6 without gestational success.
Conclusions: Although the number of mobile spermatozoa was decreased, they retain the ability of fertilization and producing viable embryos. Since it is no longer necessary to purchase a new semen donor straw, the final cost of 02 IV treatments is reduced. New tests should be conducted expanding the number of cases.
P-60. The reproductive profile of patients undergoing genetic analysis
Caio P Barbosa1,2, Monise C Santos1,2, Camila M Trevisan1,2, Bianca Bianco1,2, Denise M Christofolini1,2
1Instituto Ideia Fértil
2Faculdade de Medicina do ABC
Objective: Embryo genetic analysis techniques have been shown to increase the chances of pregnancy in patients with different causes of infertility. However, the results obtained for each cause cannot be generalized. The objective of this study was to observe the success rates obtained for each group of patients.
Methods: The study included 675 ovules fertilized by ICSI and 166 embryos evaluated by PGD-PCR, CGH-array, SNP-array and NGS. Reproductive variables evaluated were fertilization rate, embryo cleavage rate, blastocyst formation, and embryo euploidy. These variables were correlated with maternal age indications, implantation failure, chromosomal translocations, several chromosomal abnormalities, diseases genetic, severe male factor and recurrent abortion. Data was statistically analyzed by chi-square test and results were considered statistically significant when P<0.05.
Results: Was observed that patients with chromosomal translocation and male factor have higher(75%) and lower(50%) fertilization rate respectively, P<0,001. The male factor indication have a higher rate of blastocyst formation(83%) and the lowest rate is present in the implementation failure indication(28%), P<0,001. Regarding the presence of euploid embryos, patients indicated for male factor have higher rates of euploid embryos(66%) and implantation failure and repeat abortion have higher rate of aneuploidy(83% for both), P<0,001.
Conclusions: We conclude that among the indications of PGD / PGS better results are obtained in cases of male factor. In cases of translocations and repeated abortions there is good fertilization and cleavage, but there is large number of aneuploid embryos. When starting treatment, patients may be informed of the statistical probabilities within each indication plan in accordance with their reproductive expectations.
P-61. The impact of immature oocytes quantity on the rates of fertilization, cleavage, embryo development and total pregnancy in ICSI cycles
Juliana Polisseni1, Carolina M de Assunção1, Fernanda Polisseni1, Josélio V Rosa1, Jociane V S Oliveira1, Larissa M Coutinho1, João P J Caetano1
1Pró-Criar Medicina Reprodutiva, MG, Brazil
Objective: The goal was to evaluate the effect of the number of retrieved immature oocytes on rates of fertilization, cleavage, discarded embryos and total pregnancy in ICSI cases.
Methods: A retrospective study was performed at Clinical of Reproductive Medicine in Zona of Mata Mineira, from January 2015 to April 2016. The inclusion criterion for the study was ICSI cycles that the patient age was ≤36 years old and used long protocol for ovulation induction, for minimize the influence of others factors on implantation capacity. Patients were divided into groups: A with 1-2 immature oocytes (N=20) and B with more than 2 immature oocytes (N=42). For rates of fertilization, cleavage and number of discarded embryos, were compared with Student’s t test as mean±SEM (P<0.05). Chi-square test (P<0.05) was used to compare total pregnancy rates.
Results: The number of oocytes retrieved, rates of fertilization and cleavage were, in group A, (14.3±2.08; 0.81±0.03; 0.99±0.01) and group B (17.69±0.94; 0.87±0.02; 0.98±0.01), respectively. The total pregnancy was 55.0% (11/20) in group A and 35.7% (15/42) in group B. There was no significant difference between groups (P>0.05). However, for discarded embryos, the group A (2.80±0.83) had average significantly lower (P<0.05) than group B (4.83±0.42).
Conclusions: To maximize the ICSI success rates, the number of MII oocytes in stimulated cycles is important. Our study suggested negative impact of immature oocytes on early embryo development. However, the influential effects of immature oocytes in ICSI are still unclear and were necessary more studies with large sample size to elucidate.
P-62. Use of subcutaneous granulocyte colony stimulating factor (Filgrastine®) in ICSI procedure and fresh embryo transfer, for patients with reference to the age group less than or equal to 40 years old, regardless of endometrial thickness measure
Rodopiano S Florencio1, Mylena N C Rocha1, Corival L A de Castro1, Fernando C Santos1, Marta C C F Finotti1, Eduardo C Castro1, Vinicius A de Oliveira1
1Humana Medicina Reprodutiva Goiânia/ GO, Brazil
Objective: To determine the chance of pregnancy for ICSI patients with reference to the age group less than or equal to 40 years old, regardless of endometrial measure in patients using or not subcutaneous Filgrastine® 300 on the day of eggs collection.
Methods: One hundred ninety eight patients undergoing ICSI procedure, from 2013-15, including low (1-3 ovules), normal (4-12 ovules), or high ovarian reserve (> 12 ovules) took part in the study. The procedure was performed by the same professional in all clinical phases (accounting for 22% of all procedures during this period). We offered the experimental use of subcutaneous Filgrastine® 300, based on a single dose on the day of egg collection and after the procedure was performed. The patients authorized the publication of the results through informed consent. The group of patients included those with 1- 7 embryo transfer with any clinical indication, subjected to ICSI and fresh embryo transfer. Patients receiving fresh or frozen eggs were excluded. All patients with indication for IVF/ICSI after the clinical investigation were submitted to ovulation induction with gonadotropin recombinant or not, associated with LH or not, at a daily dose of 150 to 300 IU sc. from the 2nd day of the cycle. The microdose GnRH agonist was used as an adjunct to gonadotropin therapy in a long-acting GnRH regimen, associated to birth control pill in the previous cycle or with GnRH antagonists for patients with dominant follicles 13-14mm. Patients received Ovidrel® 250 or Lupron Kit 0.4 ml sc for the final follicular maturation. Luteal phase maintenance was performed with oral or patch estrogen, vaginal or intramuscular progesterone or low Ovidrel® doses, depending on the drug used for the final follicular maturation. The experimental group(using Filgrastine®) comprised 89 patients and the control group 109 patients. In each group, we assessed the average age, previous ICSI cycle number (including the current one), day and type of embryo transfer (1, 2, 3 or 4). We considered type 1 being the best embryo transfer. The endometrial layer was measured in millimeters on the final maturation day.
Results: The experimental group showed no statistical difference regarding the average of the following variables that could interfere with the likelihood of pregnancy: average age (33,76/33,61; P=0.391); type of embryo transfer (1,48/1,48; P=0.469) and endometrial thickness measure (10,52/10,65; P=0.342); however, there were statistical difference regarding the number of previous cycles (2,01/1,63; P=0.014) and the transfer day (3,71/3,96; P=0.013). The experimental group showed a clinical pregnancy frequency of 34.8% versus 30% in the control group, P=0.482.
Conclusions: There was no statistical difference in the chance of clinical pregnancy, but the experimental group had a greater number of previous cycles and earlier egg transfer which was statistically significant. Thus, further studies with more defined groups and with patients showing implantation failure will better assess the usefulness of this subcutaneous drug and the chance of pregnancy, regardless of endometrial thickness measure.
P-63. Ethics involved on fertility preservation for pediatric cancer patients: review and discussion
Irislande Inácio1, Fernando Castelo Branco1, Bruno Ramalho De Carvalho3, Jhenifer Kliemchen Rodrigues1,2,3
1Associação Instituto Sapientiae, São Paulo/ SP, Brazil
2In Vitro Consultoria, Belo Horizonte/ MG, Brazil
3Latin America Oncofertility Network - Oncofertility Consortium
Objective: Improved survival rates of pediatric and adolescent cancers, increased attention on the discussion about quality of life after treatment. Ethical thinking around fertility preservation (FP) procedures for children and young cancer patients is essential at this time. There is an increasingly pressing need to discuss the ethics of failing to preserve fertility, particularly for groups for whom established techniques exist. Discussing oncofertility, cancer treatment’s possible effects on FP options, means to address this concern by informing patients and parents regarding options available to prevent future struggles with infertility. This literature review and discussion aimed to summarize attitudes, beliefs, and patterns of behavior of patients, parents, and healthcare providers in oncofertility when children or adolescents are involved, through a bibliographic survey involving preservation of gametes in pediatrics patients.
Methods: A literature survey was conducted in books and online databases on the ethical dilemmas involved on fertility preservation for pediatric cancer patients.
Results: Reports and papers on the theme were found in literature, supporting the concept that adolescents and their parents have similar informational and counseling needs. Both seek to be fully informed about cancer treatment’s effects on fertility and FP options. Also, parents and healthcare professionals sometimes underestimate the importance of fertility for the future of infants and adolescent cancer patients.
Conclusions: In order to overcome discussion barriers and meet pediatric patients and their parents’ informational needs, it is essential to create and implement practice guidelines, as well as properly educate and train healthcare professionals about oncofertility issues.
P-64. The use of erotic visual stimuli during semen collection according to the purpose of the sample
Beatriz M Silva1, Eduardo S De Araújo1, Frederico J S Correa1, Isadora S Chaussard1
1FERTIL CARE - Centro de Reprodução Humana, Brasília/DF, Brazil
Objective: This study aimed to correlate the individual choice by erotic visual stimulus during the seminal collection versus purposes of the semen samples.
Methods: Among 222 patients who collected semen in the clinical facilities, 216 patients answered to the questionnaire, indicating their choice to have or not to have erotic visual stimulus (video) during the collection, were included in the survey. They were separated into two groups. Group A (N= 133) would have seminal sample used for investigative purposes (spermiogram/seminal prognosis test/sperm DNA fragmentation) and group B (N=83) would have sample intended for procedure purposes (insemination/IVF/cryopreservation for fertility preservation).
Results: The preference for visual stimulation during the seminal collection among investigative purpose was 68.42%, while for insemination or fertilization was 52.80%. With the analysis Chi-square statistics, it was observed difference statistically significant between groups A and B (P = 0,00229) considering difference P<0,5.
Conclusions: The final destination of the sample interferes with the patient’s choice by visual stimulus at the time of collection, it may be related to psychological, emotional and even religious factors inherent in each individual, since the correlations A x B showed differences statistic. Finally, we believe that clinics should continue promoting the well being of the patient by offering this option of choice prior the seminal collection making it the most comfortable and custom procedure.
P-65. Evaluation of assisted reproduction services in the city of Ribeirão Preto/SP
Wellington Sanches1, Fabiana P N Nogueira1, Margareth J Dias2
1Divisão de Vigilância Sanitária da Secretaria Municipal da Saúde de Ribeirão Preto/ SP, Brazil
2Grupo Técnico Estadual de Vigilância Sanitária de Ribeirão Preto/ SP, Brazil
Objective: To analyze the health risk of the six assisted reproduction services in the city of Ribeirão Preto (one public and five private).
Methods: This study was carried out by technicians of the Municipal Division of Health Surveillance and by the Health Surveillance Group XXIV - Ribeirao Preto Region. It was used descriptive analysis of secondary data from 9 Health Inspection Scripts in Reproduction Banks [proposed by the Brazilian Health Surveillance Agency (ANVISA)], containing a total of 101 single choice questions, which allowed the following three possible responses “yes”, “no” and “not applicable”, considering the level of criticality proposed by the script (I, II and III). The modules investigated were general documentation (25 questions), physical infrastructure (8 questions), patient/donor screening (10 questions), processing samples (48 questions) and quality assurance system (10 questions). They were used in nine inspections for 18 months, from November 17, 2014 to May 19, 2016. Three services were inspected only once and one of them was not working and waiting for the initial Operating License.
Results: In one of the services, the risk rating increased because of inadequate physical structure of some environments while in the other, the highest risk factor was the screening of donors. In the nine inspections, it was verified that four services meet 100% of the requirements of the script regarding physical structure, one meets 91.69%, and one meets 61.11%. Regarding the screening of donors, four services meet 100% of the requirements, one meets 82.76% and one did not perform the procedure until the time of the inspection, and for this reason, it could not be evaluated in this parameter.
Conclusions: the highest risks are related to the inadequacy of the physical structure and to not performing the repetition of donor screening tests. The physical structure of the service should meet the current legislation, and the screening of donors must occur strictly and with special attention to critical levels, minimizing health risks in assisted reproduction services.
P-66. Supraphysiological concentrations of gonadal hormones reduce the anxiety behavior in female rats submitted to psychogenic stress
Luciana Le Sueur-Maluf1, Flora F N Mariotti1, Giovanna Pimpão1, Hanna K M Antunes1, Augusto A de Melo1, Heloísa A Baptista1, Milena B Viana1, Isabel C Céspedes1
1Universidade Federal de São Paulo – UNIFESP, SP, Brazil
Objectives: We aimed to evaluate the effect of supraphysiological levels of gonadal hormones on the induced-stress response in female rats.
Methods: In order to mimic the context of ART in rodents, female Wistar rats were submitted to the superovulation protocol (150 IU/Kg of eCG and 75 IU/Kg of hCG) and then to psychogenic stress (induced by restraint for 30 minutes during three days). Four groups were tested: Superovulation/Stress group (SOS; n=10): submitted to superovulation and restraint stress; Superovulation group (SO; n=10): submitted only to superovulation; Stress group (S; n=10): submitted only to the restraint stress; and Sham group (Sh; n=10): not exposed to superovulation nor stress. The anxiety behavior was evaluated in the elevated plus-maze (EPM) and validated in an open field test. The corpora lutea was counted as an indication of superovulation efficiency. The results were compared using ANOVA or Kruskal-Wallis test and expressed in Media+SE (P≤0.05).
Results: Significant increase in the number of corpora lutea was observed in the SO group (71.83±8.68) and SOS (75.00±5.43) compared to Sham (31.71±3.16) and S (33.11±3.00). EPM showed a significant decrease in time spent by S group in the open arms (7.11±2.05 sec) and an increase in time spent in the closed arms (92.89±2.05 sec) compared to Sham (20.00±3.57 sec and 79.56±3.49 sec, respectively). Those effects were not observed in the SOS group.
Conclusions: Our findings suggest a protective (anxiolytic) effect of high levels of gonadal hormones on the stress response in female rats.
P-67. Equipment for concentration and comparative motility sperm
Regina A A Navogino1
1Setor de Analise Seminal Grupo Fleury Medicina e Saude, Brazil
Objective: Compare the SQA-V GOLD (SQA-V), equipment used for human semen analysis to the current method, Hamilton Thorne (HT) equipment, using concentration and motility results obtained in routine semen clinical analysis. The results from both equipments were controlled by the Neubauer chamber manual analysis (NC), the gold standard method for human sêmen analysis.
Methods: The HT is a semi-automated equipment and operates as a motion cell analyzer. Using microscope, with a heated platinum, to capture sequential images and obtain the concentration and motility of spermatozoids.
The SQA-V equipment with an automated system that also analyze concentration and spermatozoid motility using an electro-optical detection technology based on algorithms that follow standardized values by WHO. The NC analysis method is based on counting spermatozoids to concentration and for motility; 10uL of material is analyzed in a lamina covered with cover slip viewed in optical microscope. The samples were randomly obtained from 01/07/2015 to 31/07/2015. All oligozoospermics and azoospermics semen samples were excluded. The human semen analysis results of concentration and motility were compared between the methods: HT compared to NC and SQA-V compared to NC
Results: The HT concentration analysis results were 95% equivalent to NC and the SQA-V results were 30% equivalent. The HT motility results were 100% equivalent to NC results and the SQA-V were only 12% equivalent.
Conclusions: Considering the concentration and motility, the SQA-V equipment results showed lower percentage concordance compared to NC than the HT results analysis in this group of patients studied.
P-68. Adding the number of follicles 14-16mm to hCG trigger criteria makes a difference?
Ana Márcia M Cota1, Márcia C F Ferreira1, Moísa L Pedrosa1, Bruna O Martins1, Rívia M Lamaita1, Márcia M Carneiro1
1Reprodução Humana Mater Dei, Belo Horizonte/MG, Brazil
Objective: Traditional criterion to trigger ovulation in IVF cycles has been at least two follicles > 17mm. This study aimed at evaluating whether adding the number of follicles 14-16mm (F14-16) on the day of hCG would improve oocyte yield and maturity status.
Methods: We retrospectively analyzed 118 consecutive IVF cycles data regarding age, numbers of follicles > 17 mm, F14-16, oocytes, MII (mature) oocytes, MI (first division of meiosis) oocytes and GV (germinative vesicle) oocytes. Patients were assigned in either Group 1 (those with 3 or more F14-16) or Group 2 (less than 3 F14-16). Data were analyzed using SPSS, with P <0.005 considered statistically significant.
Results: Results are shown in the table below, as mean ± standard deviation.
Conclusions: Adding the number of F14-16 on the day of hCG trigger did not improve oocyte yield or the number of mature oocytes but increased the number of GV oocytes.
P-69. Psychological profile of pacients seeking tertiary care of infertility
Ana K Bartmann1, Lucas L M da Silva1, Amélia G V de Melo1, Paulo C Saran1, Uebe C Rezek1
1Universidade de Ribeirão Preto - Clínica Ana Bartmann
Objective: To investigate, through a questionnaire, the psychological and social aspects of infertile patients attended at the Infertility Ambulatory Clinic of Electro Bonini Hospital, in the city of Ribeirão Preto/ SP.
Methods: 116 women who sought care for investigation and treatment of infertility were interviewed. The results were analyzed to identify the psychological profile of the patients.
Results: The main questions took into account the degree of sadness for not getting pregnant, their hope to get pregnant, if they had already been pregnant, if they had ever thought about adopting a child, withdrawal of treatment. The results were consistent with the data found in the literature. The biopsychosocial profile analysis revealed a strong degree of sadness and prejudice or social pressure for not getting pregnant. However, those women have great hope of getting pregnant and the vast majority doesn’t think of quitting treatment.
Conclusions: This study proves the pathological aspect that infertility causes in the lives of couples, especially women, since 75% reported that they feel unhappy or depressed for not being able to get pregnant. Multidisciplinary work, in that sense, plays an important role in understanding the intimate and deep emotional conflicts that infertility causes.
P-70. Implementing the nursing service in a new center for human reproduction
Giselle S Dias1, Beatriz M Silva1, Frederico J S Correa1
1FERTIL CARE - Centro de Reprodução Humana, Brasília/DF, Brazil
Objective: To report the experience of implementing the nursing service in a new center of human reproduction.
Methods: Experience report on the implementation of the nursing service in a new center of human reproduction from May to October 2015. The process was coordinated by a human reproduction trained nurse altogether with the medical and embryology team.
Results: Report described on the nurse’s point of view that joined a team composed by a nurse, a nursing technician and a nursing assistant. The center of human reproduction opened in May 2015, designed by the desire of experienced professionals and the need for a new model of care to infertile couples. The process of implementation of the nursing service was divided into three fronts. The first was to observe and define the operational area of the nursing team, analyzing whether professionals perform their activities as described in the Law of N. 7.498 of06.25.1986 according to the regulation of nursing practice. The second was specific training team focused on human reproduction. Finally, the standard operating procedures were discussed and implemented.
Conclusions: Human reproduction is a health service of high complexity involving ethical and humanistic aspects, it is essential to have nurses trained in the field, being perfectly feasible the implementation of the nursing service.
P-71. Cognitive behavioral therapy: assisted human reproduction in women
Bruna R de Marchi1, Cássio L Fácio1, Ligiane A M de Paula1, Ligia F Previato1, Edilberto Araujo Filho1
1Centro de Reprodução Humana de São José do Preto (CRH-Rio Preto), São José do Rio Preto/ SP, Brazil
Literature Review: Infertility is defined as absence of pregnancy after one year of regular sexual intercourse without use of contraceptive methods. In women undergoing treatment for Assisted Human Reproduction (AHR), stress related to infertility is more expected, related to the fact of capacity of woman conceive a child. This literature review aimed to determine the effectiveness of CognitiveBehavioral Therapy (CBT) in women submitted to treatment by Assisted Human Reproduction (AHR). The research method was Google Scholar, Scielo and Pepsic, using the keywords: cognitive-behavioral therapy and assisted human reproduction; cognitive-behavioral therapy and infertility in women; cognitive-behavioral therapy; infertility in women; human reproduction assisted. It were included articles found in databases, those cited in other relevant reviews and publications associated with the intervention of CBT in AHR, totalizing 55 articles. Of these, 28 articles were written using english language, and 27 using portuguese language. The articles related anxiety, stress and depression as a common symptom in women undergoing AHR treatment. The CBT was efficient and appropriate in the treatment of these symptoms associated in women undergoing AHR.
P-72. A case report supporting the concept that some women have a predisposition for maternal meiosis erros
Juliana Polisseni1, Carolina M de Assunção1, Fernanda Polisseni1, Josélio V Rosa1, Jociane V S Oliveira1, Larissa M Coutinho1, João P J Caetano1
1Pró-Criar Medicina Reprodutiva, MG, Brazil
Introduction: A case report of recurrent triploidy of maternal origin after ICSI was performed, eliminating the possibility of the most common etiology for an addition set of chromosomes whiches the penetration of the oocyte by two sperm.
Case Report: A 37-year-old woman had a ICSI cycle in 2014 and 2015 with 100 percent of oocytes triploidy. Also chromosome analyses on the bolth the female and male partner were normal (46XX, 46XY). In 2016 another cicle was performed using semen of partner and donated oocyte. In ICSI cycle utilizing donated oocyte all the fertilization was normal, with embryos with good quality.
Comments: One of the most common mechanisms involved in triploidy of maternal origin in non-extrusion of the second polar body. One possible explanation for tetraploid embryo was the combination of two female pronuclei wih pronuclei of male. Thus, there would also have to be a maternal meiosis error with failure to extrude the second polar body.
P-73. A prospective study comparing two embryo transfer soft catheters
Emily de Conto1,2, Artur K Schuster1, Vanessa K Genro2, Rita de Cassia B Chapon1,2, Daniela S da Silva1,2, Joao S da Cunha-Filho1,2
1UFRGS - Universidade Federal do Rio Grande do Sul, Porto Alegre/ RS, Brazil
2Insemine - Centro de Reprodução Humana, Porto Alegre/ RS, Brazil
Objectives: to correlate the efficacy of Set TDT® and Cook® Sydney IVF soft catheters for reproductive outcomes of assisted reproductive technology cycles. The primary outcome was defined as positive β-human chorionic gonadotrophin (β-hCG) test.
Methods: this is a prospective study that recruited 68 patients undergoing in vitro fertilization and intra-cytoplasmic sperm injection cycles in a private fertility clinic in Porto Alegre, Brazil, between January 2014 and April 2016. They were divided into three groups according to the catheter that would be used for the embryo transfer and groups were matched for age. The total of patients in each group was: 34 for TDT and 34 for Cook Sydney IVF. All the patients were submitted to a β-hCG test 12 days after the embryo transfer for pregnancy outcome evaluation.
Results: 10 out of 34patients of TDT group had a positive outcome for pregnancy, corresponding to 29%. The Cook Sydney IVF group had 9 patients out of 34 with positive outcome, corresponding to 26%. Comparing the efficacy of both catheters for primary outcome, there was no significant difference (P > .05) between TDT and Cook Sydney IVF catheters.
Conclusions: the efficacy of TDT and Cook Sydney IVF catheters are similar for embryo transfer during assisted reproductive technology cycles.
P-74. Embryo stage of development is not decisive for reproductive outcomes in frozen-thawed embryo transfer cycles
Bruno R de Carvalho1, Marina W P Barbosa1, Helena Bonesi1, David B Gomes Sobrinho1, Iris O Cabral1, Antônio C P Barbosa1, Adelino A Silva1, Jose R Iglésias1, Hitomi M Nakagawa1
1Genesis - Center for Assistance in Human Reproduction, Brasília/ DF, Brazil
Objective: To evaluate if the outcomes of IVF/ICSI in frozen-thawed embryo transfer and fresh embryo transfer cycles differ according to cleavage and blastocyst stages.
Methods: Retrospective cohort study to compare IVF/ICSI outcomes between fresh embryo transfer and frozen-thawed embryo transfer cycles, according to the stage of embryo development. Analysis was carried out on 443 consecutive embryo transfer cycles performed between January 1st and December 31st, 2014. Women aged up to 38 and submitted to embryo transfer cycles with fresh (n=309) or frozen-thawed (n=134) embryos at a private center for assistance in human reproduction were considered for analysis. In each group were stratified according to the stage of embryo development: cleavage stage and blastocyst stage. Main outcome measures were implantation rate, clinical pregnancy rate, ongoing pregnancy rate and live birth rate per cycle.
Results: In fresh embryo transfer group, for cleavage stage versus blastocyst stage, respectively, implantation rates were 22% and 47% (P=0.0005), clinical pregnancy rates were 34% and 64% (P=0.0057), ongoing pregnancy rates were 30% and 61% (P=0.0046) and live birth rates were 28% and 55% (P=0.0148). There were no significant differences in those rates between cleavage and blastocyst stages in frozen-thawed group, neither between fresh and frozenthawed cleavage embryo transfers nor between fresh and frozen-thawed blastocyst transfers.
Conclusions: Our results confirm that blastocyst transfer is better than cleavage stage in fresh embryo transfer cycles. In frozen-thawed cycles, cleavage or blastocyst stages seem to offer similar reproductive outcomes.