JBRA Assisted Reproduction 2013; 17 (6):340-343
ORIGINAL ARTICLE
doi: 10.5935/1518-0557.20130076
Introduction of the method of intravaginal culture (IVC), through the device INVOCell routine laboratory RHA in Brazil
Introdução do método de cultura intravaginal (IVC), através do dispositivo InVOCell em rotina de laboratório de RHA no Brasil
1 Centro de Infertilidade e Medicina Fetal do norte Fluminense. Hospital Escola Álvaro Alvim
2 Centro Colombiano de Fertilidade e Esterilidade - CECOLFES
Trabalho executado no Centro de Infertilidade e Medicina Fetal do norte Fluminense. Hospital Escola Álvaro Alvim.
RESUMO
Introdução: A fertilização in vitro convencional e a microinjeção intracitoplasmática de espermatozóides são atualmente as técnica estabelecidas para o tratamento de infertilidade, porém na ultima década o processo de fertilização in vitro tem sofrido diversas modificações na indução de ovulação e recuperação de oocito (Ranoux 1990, Seibel 1988; Ranoux, 2008). O procedimento INVO tem sido utilizado no tratamento de pacientes com diferentes causas de infertilidade em vários paises. Esse é um procedimento desenvolvido a mais de 20 anos e é uma alternativa simples e de menor custo para o tratamento de infertilidade comparada a técnicas convencionais. Um achado interessante desta técnica de cultura intravaginal são os benefícios fisiológicos e a redução do número de etapas de manipulação diminuindo o risco de contaminação.
Objetivo: Esse estudo teve como objetivo avaliar a possibilidade de incluir o método INVO através do uso do dispositivo INVOcell™ na rotina de laboratórios de tratamento de infertilidade conjugal. Que por sua vez tende a proporcionar a simplificação do trabalho laboratorial e com isso a redução dos custos de um tratamento de infertilidade.
Materiais e Método: Participaram desse estudo 40 mulheres que foram tratadas no serviço de Reprodução Humana do Hospital Escola Álvaro Alvim, no período de Agosto de 2011 a Janeiro de 2012. A todas se utilizou o protocolo de estimulação ovariana MILD modificado. O numero de pré-embriões transferidos para a cavidade uterina seguiu a Resolução CFM nº. 1.957/10.
Resultados e Conclusão: Não houve diferença significativa nos resultados apresentados pelo dispositivo INVOcell™ mostrando que o mesmo pode ser incluído em rotina de laboratório de reprodução humana assistida.
Palavras Chave: Cultura Intravaginal, FIV, Estimulação Ovariana
ABSTRACT
Introduction: The conventional in vitro fertilization and the intracytoplasmic sperm microinjection are currently the established techniques for the treatment of infertility. In the last decade, however, the process of in vitro fertilization has suffered several changes in ovulation induction and oocyte retrieval (Ranoux 1990, Seibel 1988; Ranoux, 2008).
The INVO procedure has been used to treat patients with different causes of infertility in many countries. This is a procedure which was developed over 20 years ago and is simpler and less costly to the infertility treatment when compared to conventional techniques. Interesting finding of this intravaginal culture technique are the physiological benefits and the reduction of the number of handling steps, reducing the risk of contamination
Objective: This study aimed to evaluate the possibility of including the method INVO through the use of the device INVOcell™ in routine laboratory treatments of couple infertility. That, in turn, tends to provide the simplification of laboratory work and thereby reduce the costs of infertility treatment.
Material and methods: 40 women were included in this study, who were treated at the Service of Human Reproduction School Hospital Álvaro Alvim, in the period from August 2011 to January 2012. On all of them it was used the protocol of modified mild ovarian stimulation. The number of pre-embryos transferred into the uterine cavity followed the CFM Resolution nº. 1.957/10.
Results and conclusion: There was no significant difference in the results presented by the device INVOcell™. Therefore showing that it can be included in routine laboratory assisted human reproduction.
Keywords: Intravaginal Culture, IVF, ovarian stimulation.
INTRODUCTION
Since the last decade, the process of in vitro fertilization (IVF) has undergone several modifications in the induction of ovulation and oocyte retrieval (Seibel Ranoux & 1990 & Seibel et al. 1988). The conventional in vitro fertilization (IVF) is now an established treatment for infertility (Ranoux, 2008). This is an assisted reproduction technique which consists in placing, in a laboratory environment, in vitro, a significant number of sperm around each oocyte (female germ cell), seeking pre-embryos of good quality will be transferred later to the uterine cavity. The intravaginal culture (IVC) of gametes, also called INVO is a procedure developed more than twenty years ago (Ranoux et al.1988), but due to problems such as contamination of the culture medium, reported with its prototype, made cease its use for some years. The new device INVOcell ™ (figure 1) technology has been improved to become an alternative simple and with less cost for the treatment of infertility compared to conventional IVF. The INVO procedure has been used to treat patients with different causes of infertility. The INVO technique consists of fertilizating oocytes and early incubation of pre-embryo in a plastic device, called INVOcell ™, hermetically closed, however permeable to O2 and CO2, and which maintains the pH within the medium. This device is balanced with the gas vaginal epithelium making the vagina generating system of CO2 and O2 reducer with proper moisture and temperature causing the vagina of the patient to act as an incubator. (Ranoux & Frydman, 2008). Interesting findings of IVC technique are physiological benefits and reduced number of handling steps that reduce the risk of contamination. (Ranoux & Seibel 1990). The procedures performed in assisted reproduction treatment entail, in general, changes in emotional aspects of patients, including an impact on daily life thereof. These impacts are negative, requiring systematic psychological. However, the device INVO offers the patient a more personal approach to achieve pregnancy, resulting in greater security and reducing anxiety levels and is considered one of the benefits of this method. One of the main advantages of using this device is the fact that the patient is allowed the opportunity to actively participate in the process of fertilization. (Ranoux & Seibel 1990). This treatment promotes well-being for women, increasing self-esteem. It was observed that stress is present in women experiencing infertility treatment, however, suggests that while the method INVO stressor, compared to conventional IVF method yielded better results in not trigger stress. According to publications of technical studies related to IVC clinical pregnancy rates ranging from 19.6% to 31%. (Ranoux, 1988 and 1990; Bonaventura. et al.2006). Based on this information we began a preliminary study published nonrandomized in our laboratory.
This study was combined with the technique INVO ovarian induction, using the ovarian stimulation protocol MILD modified. The stimulation protocol MILD recruits a small number of follicles in which a small amount of oocytes are recovered. (Frydman Ranoux & 2008).
Teramoto and Kato in 2007 observed that the incidence rate of the LH surge decreased when clomiphene citrate was administered over 5 days, which was the usual procedure. This study indicated that there may be a third method than the conventional method using induction ovarian GnRHa or GnRH antagonist. It was thought that this new method could be revolutionary in that it could prevent premature LH surge, maintaining the functions of the hypophysis, unlike the conventional method, which inhibits pituitary function. The stimulation mild protocol recruits a small number of follicles in which a small amount of oocytes are recovered (Frydman Ranoux & 2008). According Bart et al, 2010, Branigan and Estes, 2000 mild ovarian stimulation can be defined as a method where there HMG and FSH administration in lower doses and / or for a few days in cycles co-treated with GnRH antagonist or when the compounds are oral used (anti-estrogens or aromatase inhibitors), either alone or combined with gonadotropins in order to limit the number of oocytes obtained for less than eight. Another objective of the protocol is to develop a more secure protocol in which the risks of treatment are minimized (Diedrich and Ferberbaum, 1998; Olivennes and Frydman, 1998; Fauser et al., 1999; Olivennes et al., 2002; Nargund and Frydman, 2007, Pennings and Ombelet, 2007; Ubaldi et al., 2007).
In this study we evaluated the possibility of including the method by using the INVO INVOcell ™ device as another treatment option in routine laboratories of infertility treatment aiming to provide simplification of laboratory work and thereby reducing the costs of treatment of infertility.

Figure I. Constituent parts of the device INVOcell ™.
(a) inner chamber. (b) outside chamber.
MATERIALS AND METHODS
40 women with a mean age of 34 years (29-44 years), were treated at the Service Human Reproduction at Hospital Escola Álvaro Alvim / Centro de Infertilidade e Medicina Fetal do Norte Fluminense, in the period December 2010 to May 2011 . Exclusion criteri were patients with severe male factor and those who did not agree to sign the consent form. The patients were divided into two groups: group I consisted of 20 patients in which we used the method INVO and group II consisted of 20 patients in which we used the ICSI technique. All patients used mild ovarian stimulation protocol modified by the service. We used two tablets per day of clomiphene citrate 50 mg (Clomid ® or Indux ®) 5 days associated with urinary gonadotropin 75 IU (Menopur ®) for 6 days, the pituitary was conducted with indomethacin 50 mg (Inducid ®) three times daily for 5 days, when there was an ovarian follicle of 15 mm. For luteinization of follicles it was administered one dose of 0.02 mL of 0.1 mg of leuprolide acetate (Lupron ®) (flare up) taking advantage of the endogenous LH when there was an ovarian follicle of 17 mm or more. The ovarian aspiration occurred 36 hours after administration of leuprolide acetate, employing COOK ® 17G needle under suction pressure of 120 mm Hg, guided transvaginal ultrasound probe of 7.5 mHz (Aloka 500 ® - JAPAN), with the patient sedated with 1% Propofol 10 mg / ml (Fresofol ®). From day puncture on it was administered 3 tablets a day for 14 days 200 mg of progesterone (Utrogestan ®) for luteal phase support and initial support in case of pregnancy. During ovarian stimulation “Mild modified” three examinations were performed by ultrasonography (GE ® appliance model Voluson-730 Pro) for monitoring of follicular growth. During the follicular aspiration, follicular fluid was collected in sterile tubes and sent to the laboratory where the ova were recovered, washed with modified HTF (Irvine Scientific ®) supplemented with 10% SSS (Irvine Scientific ®) (serum substitute supplement) in plate 4 wells and sorted according to quality of cumulus-oocyte complex (COC). Immature oocytes or those with denerated aspects were discarded. In group I, oocytes were placed with sorted sperm for fertilization technique enabled by the swim-up, diluted in a concentration of from 30,000 to 50,000 sperm per ml in culture medium (SSM ® Irvine Scientific) with 10% SSS (Irvine Scientific ®) inside the device INVOcell ™ immediately. Then the device was deposited INVOcell ™ vaginal cavity. The removal of the device took place 72 hours after. The INVOcell was then removed™, washed with saline at 37 ° C, and the culture medium contained in the device was analyzed for the removal of the embryos. Embryos produced within the INVOcell ™ plates were transferred to one well and transferred. In group II, the technique applied was ICSI. The transfer was carried out using transfer catheter SURE ®-PRO ULTRAtm WALLACE coupled to a 1 ml syringe and a Terumo ® disposable speculum. The number of pre-embryos transferred to the uterine cavity followed the resolution of the Brazilian Federal Council of Medicine (CFM paragraph. 1.957/10).
RESULTS
40 cycles were performed, with an average patient age of 34.5 years (Table I) using ovarian stimulation protocol mild modified, of which 20 took place and the INVO technique that did not fit the inclusion criteria underwent intracytoplasmic microinjection sperm injection (ICSI).
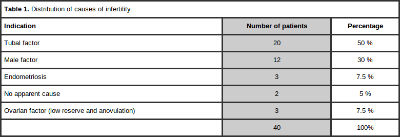
Table 1. Distribution of causes of infertility
According to Table 1, 50% had clinical indication as tubal factor, these 100% INVO technique were used. We excluded couples with severe male factor (30%), ovarian factor (7.5%) and unexplained infertility (5%), which was used in the ICSI technique.
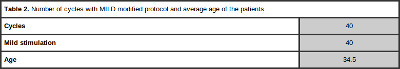
Table 2. Number of cycles with MILD modified protocol and average age of the patients
In the 20 INVO cases, was recovered after follicular aspiration an average of 4:10 oocytes, 3.68 ranked as metaphase II, according the expansion of complex cumulus oocyte (table III). There was 1 cycle of failed fertilization and 19 cycles of fertilization, and we obtained an average of 2.42 pre-embryos that exhibited a rate of 86.66% with no or up to 20% of fragmentation (Grade 1 and Grade 2) and fragmentation with 13.34% greater than 20% (Grade 3 and Grade 4 ). With an average of 1.89 pre-embryos transferred in 18 cycles.
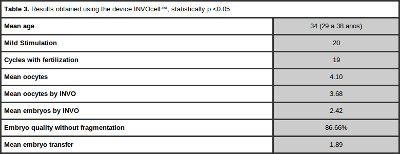
Table 3. Results obtained using the device INVOcell™, statistically p <0.05
In the 20 cases that did not meet the inclusion criteria was performed ICSI technique (Table IV). The average number of oocytes retrieved was 3.2 oocytes, and the media used (metaphase II) of 2.9 per cycle. There was no failure of fertilization and this group were transferred into media 2:25 pre-embryos being 87.87% with no or up to 20% of fragmentation (Grade 1 Grade 2 +), 12.13% with greater than 20% fragmentation (Grade 3 and Grade 4). With an average pre-embryos replaced was 1.6.
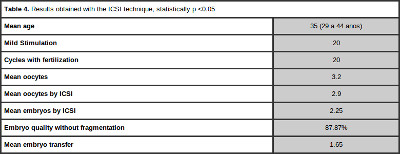
Table 4. Results obtained with the ICSI technique, statistically p <0.05
In the group that performed the method INVO , were transferred in 18 cycles and 6 patients had a positive test and clinical pregnancy. Among these 1 case evolved to abortion in the 7th week. According to Table V, in this group the clinical pregnancy rate per cycle was 30% and the clinical pregnancy rate per transfer was 33.33%. These data may be indicative of the efficiency of this method, besides not presenting cases of multiple pregnancy.
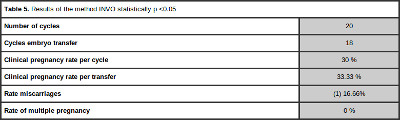
Table 5. Results of the method INVO statistically p <0.05
According to the results shown in Table VI, among the ICSI cycles, there were transferred embryos in all cycles, resulting in a clinical pregnancy rate per cycle and per transfer of 25% and one case of abortion.
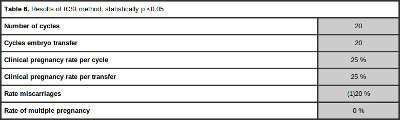
Table 6. Results of ICSI method, statistically p <0.05
As statistical tests performed with the results of Tables III, IV, V, VI we calculated a confidence interval and performed a hypothesis test for the difference of proportions according to the relations of the data related to the quality of the embryos, we obtained a range of 95% and a margin of error of 5% noted that the two techniques no significant difference (α = 0.05) with respect to embryo quality. Regarding Tables V and VI was observed that there was no significant difference (α = 0.05) in relation to clinical pregnancy rates per transfer which demonstrates that the INVO technique can be used.
DISCUSSION
The purpose of this preliminary study was to evaluate the possibility of including the method by using the INVO INVOcell ™ device as another treatment option in routine laboratories marital infertility treatment. In our study there was no INVO method comparison with other known techniques, the method is just being presented , while ICSI was used for couples who have not entered the inclusion criteria. The INVO procedure is an assisted reproduction technique and has been used to treat patients with different causes of infertility, among them, tubal factor, endometriosis, mild male factor and unexplained infertility.
However, in our study, the indication that prevailed for the INVO technique was tubal factor. In cases where there was severe male factor ICSI technique was indicated. In this study the mild modified stimulation protocol was used for ovulation induction. The mild modified protocol is short and simple, making it more physiological, requiring less monitoring and in turn reducing all potential risks of medical complications for the patient, with no cases of ovarian hyperstimulation in the study. Currently ovarian hyperstimulation corresponds to 1% of complications in assisted reproduction treatment. (De Sutter P. et al. 2008). With their use there was a reduction in the number of oocytes retrieved, and greater synchrony follicle reducing the number of immature oocytes, the number of pre-embryos transferred and cryopreserved. The INVOcell ™ is a device that provides the balance of gases in the culture medium, because gas is balanced with the vaginal epithelium making vaginal cavity a system generator reductant O2 and CO2, and to maintain the thermal equilibrium making vaginal cavity the patient an incubator. (Fukuda et al. 1996). We can assign thermal equilibrium and gas offered by the vaginal cavity, the low rates of fragmentation of pre-embryos obtained in our study, compared to staying in conventional incubator. Our results using the device INVOcell™ associated with the mild modified stimulation protocol showed satisfactory results. These results are proven with the average of 4 oocytes retrieved per cycle, 1.89 pre-embryos transferred in media presenting 86.66% of Grade 1 and fragmentation rate de33. 33% of clinical pregnancy by transfer. Simultaneously the patients who did not fit the inclusion criteria underwent the ICSI procedure. The results were an average of 3 oocytes recovered per cycle, pre 1.6 - transferred embryos in media presented 87.77% Grade fragmentation 1 and 25% rate of clinical pregnancy by transfer. The pregnancy rate in ICSI procedure was lower due to the higher complexity of cases.
In a similar study done in partnership with the Colombian Center for Fertility and sterility – CECOLFES were performed 125 ovarian stimulation in patients with a mean age of 33.8 years. Of 114 cycles with pre-embryo transfer, there was an average of 2.4 pre-embryos transferred. Among transfer cycles, there occurred a total of 50 clinical pregnancies, abortion 11, 29 births and 10 ongoing pregnancies. This related study yielded a total of 40% of clinical pregnancy rate per egg recovered and 43.9% of clinical pregnancy rate per embryo pre-downloaded. And a multiple pregnancy rate of 20%.
As they also had no significant differences using the method INVO, it is suggested that the device INVOcell ™ may be a less invasive option, most physiological and humanized it provides the participation of the patient in treatment. Included in the routine of a laboratory of human reproduction it could provide infertility treatment with a more affordable cost.
REFERENCES
Bonaventura, L. et al. The INVOCell, a new medical device for intra vaginal fertilization and culture. Fertility and Sterility 2006; vol 86 suppl 2.
Crossref
De Sutter P., Gerris J e Dhont M. Assisted reproductive technologies: how minimize the risks complications in developing countries. Hum Reprod 2008; doi 10.1093/den 160:73-76.
Crossref
Fukuda M, Fukuda K, Ranoux C. Unexpected low oxygen tension of intravaginal culture. Human Reproduction 1996; 11:1293-1295.
Medline
Lucena E, SAA A. M, Navarro D E, Pulido C., Lombana O, Moran A. INVO Procedure:Minimally Invasive IVF as an Alternative Treatment Option for Infertile Couples. The ScientificWorld Journal Volume 2012, Article ID 571596, 6 pages doi:10.1100/2012/571596
Medline Crossref
Lucena E, SAA A. M, Navarro D E, Lombana K, Moran A. Invo Procedure: minimally invasive Ivf alternative treatment (couples). The scientific world journal,2012.
Medline Crossref
M.C. Magli, G.M .Jones, K. Lundin and E. Van den Abbeel Atlas of Human Embryology Human Reproduction Vol. 27, Suppl. 1, 2012
Medline Crossref
Ranoux C, Foulot H, Aubriot FX, Poirot C, Dubuisson JB, Chevallier O, Cardone V. A new in vitro fertilization technique: intravaginal culture. Fertil Steril 1988; 49:654-657.
Medline
Ranoux C, Seibel MM. New techniques in Fertilization: Intra vaginal culture and microvolume straw. J Vitro Fert Embryo Transfer 1990; 7:6-8.
Medline
Ranoux C, Frydman R. INVO: a simple, low cost effective assisted reproductive technology. Human Reproduction 2008; doi: 10.1093/den 163:85-89.
Crossref
Seibel MM. A new era in reproductive technology. N Engl J Med 1988; 318:828
Medline Crossref
Teramoto S, Kato O. Minimal ovarian stimulation with clomiphene citrate: a large-scale retrospective study Reproductive BioMedicine Online. Vol 15. No 2. 2007; 134-148.
Medline Crossref