JBRA Assist. Reprod. 2014; 18 (4):139-143
ORIGINAL ARTICLE
doi: 10.5935/1518-0557.20140020
Safe multidisciplinary approach in deeply infiltrating endometriosis (DIE): is it feasible?
1 Gynecology Clinic Biocor Hospital – Nova Lima/MG - Brazil
2 Coloprocotology Clinic Biocor Hospital – Nova Lima/MG - Brazil
3 Urology Clinic Biocor Hospital – Nova Lima/MG - Brazil
4 Department of Obstetrics and Gynecology, Federal University of Minas Gerais (UFMG) - Belo Horizonte/MG - Brazil
Part of this data was presented as a poster at the 11th World Congress on Endometriosis (WCE2011) in Montpellier, 4-7 September 2011.
CONFLICT OF INTERESTS
The authors declare that they have no conflict of interest.
ABSTRACT
Objective: Evaluate the type and incidence of postoperative complications after surgery for deep infiltrative endometriosis at Biocor Hospital.
Methods: Our observational study involved a multidisciplinary surgical team that performed laparoscopy on 154 patients suffering from pelvic pain. Surgical complications occurring up to the 30th postoperative day were recorded.
Results: Mean age patient age was 34.1 years. Infertility was present in 69 (45%) although 31% had not attempted to get pregnant. Dysmenorrhea was the most frequent symptom (79.3%) followed by chronic pelvic pain (59.7%) and deep dyspareunia (48,7%). Most cases required extensive surgery as the majority (n=117; 76.9%) were classified as severe endometriosis (ASRM grade IV). The most frequent surgical procedures were: 136 adhesiolysis, 100 intestinal surgeries (85 retosigmoidectomies), 92 peritonal lesion excision, 39 vaginal resections, 19 myomectomies, 21 hysterectomies and 5 partial bladder resections. Postoperative complications were recorded in 14 (9.59%) patients: 8 (5.48%) major complications and 6 (4.11%) minor. Major complications included blood transfusion (n=2) retosigmoid anastomosis dehiscence (1), rectovaginal fistula (n=1), urinary fistula (n=1), deep vein thrombosis (n=1), lower limb compartment syndrome with motor deficit (n=1) and one intestinal obstruction (n=1). Minor complications were abdominal wall infection (n=3), peripheral neuropathy (n=3), bladder atony (n=1) and bladder perforation (n=1). No deaths were observed. All major complication cases underwent retosigmoidectomy associated with vaginal resection (n=6), uterosacral ligament excision (n=5) or hysterectomy (n=3).
Conclusion: The surgical treatment of DIE is complex and subject to complications. The surgical expertise of a multidisciplinary team plays a vital role in this setting.
Keywords: Deeply infiltrating endometriosis, chronic pelvic pain, infertility, surgical complications, laparoscopy.
INTRODUCTION
Deep infiltrative endometriosis (DIE) has been defined as endometriosis that penetrates more than 5 mm under the peritoneal surface (Cornillie et al., 1990). In this situation, endometriotic implants can involve the uterosacral ligaments, the pouch of Douglas (retrocervical endometriosis), the rectovaginal septum, and even the sigmoid colon and rectum. Pain strongly correlates with the depth of the DIE lesions and the radical surgical removal of lesions remains the mainstay of treatment (Koninckx et al., 1991; Porpora et al., 1999; Fauconnier et al., 2002; Chapron et al., 2006). In this setting, the effect of medical treatments in terms of pain relief can be substantial (Vercellini et al., 2009; Mabrouk et al., 2011), but to ensure the complete removal of the disease and obtain the best results in terms of quality of life, extensive surgical removal of endometriotic lesions may be required (Chopin et al., 2005; Seracchioli et al., 2007; Darai et al., 2011; Mabrouk et al., 2011). Several published studies suggest that the complete excision of endometriosis offers good long-term symptomatic relief, especially for those women with severe or debilitating symptoms (Dubernard et al., 2006; Mereu et al., 2007; Stepniewska et al., 2009; Donnez & Squifflet, 2010; Kavallaris et al., 2011; Meuleman et al., 2012).
Treatments should be tailored to address the wishes of women according to the specific characteristics of the disease (Leyland et al., 2010; Dunselman et al., 2014). Although many questions remain unanswered, there is evidence to support the use of laparoscopic surgery to improve pain and infertility (Dubernard et al., 2006; Stepniewska et al., 2009; Donnez & Squifflet, 2010). Establishing a systematic strategy is essential to make surgery more reproducible, safer and less time-consuming. Serious complications however may arise and further interfere with quality of life (Ford et al., 2004; Fauconnier & Chapron, 2005; Seracchioli et al., 2007; Donnez & Squifflet, 2010; Fritzer et al., 2012).
Laparoscopic eradication of all visible implants is feasible and safe when surgery is performed in a referral center (Minelli et al., 2010; Fritzer et al., 2012). Unfortunately, even in the most expert hands, complications may occur and further interfere with quality of life and fertility (Donnez & Squifflet, 2010; Ford et al., 2004; Darai et al., 2007; Vercellini et al., 2007; Slack et al., 2007; Minelli et al., 2009; Kovoor et al., 2010; Kondo et al., 2011).
As endometriosis is a chronic disease an integrated approach involving a multi-disciplinary team is not just needed but fundamental. Thus a multidisciplinary surgical team led by a surgically experienced gynecologist working together in complex cases with urologists, gastrointestinal surgeons and/or general surgeons may all play an important role in providing adequate treatment and as well as increasing the likelihood of providing consistent, evidence-based and cost-efficient care (D’Hooghe et al., 2006; Simoens et al., 2012).
As our multidisciplinary surgical team has been working for over a decade (Ávila, 2008), we aimed at evaluating the type and incidence of postoperative complications after surgery for DIE Biocor Hospital.
MATERIAL AND METHODS
This observational study involved a muldisciplinary surgical team who operated on women sufferering from pelvic pain from Januray 1998 to April 2011. All surgeries were laparoscopies performed by the same gynecologist (IA) and coloproctologist (LMPC). Only cases with histological confirmation of endometriosis were included. Relevant preoperative, intraoperative, and postoperative data were retrieved and recorded in an Excel spreadsheet. Surgical complications occurring up to the 30th postoperative day were recorded.
All women underwent gynaecological examination, pelvic transvaginal and abdominal ultrasonography in order to evaluate the presence of pelvic endometriosis before surgery. Other diagnostic tests were performed when indicated, as previously described (Dunselman et al., 2014). All women were scheduled for laparoscopic management of deep infiltrating endometriosis and they gave informed written consent to surgical treatment and the possible use of their anonymous data for research purposes. The study protocol was approved the local Ethics Committee. The surgical strategy was complete laparoscopic excision of all visually suspected endometriotic lesions and the laparoscopic procedures were performed by the same surgeon (I.A.) and coloproctologist (LMPC). The surgical team had an extensive background in laparoscopic treatment of patients with DIE but we chose to evalute only one surgeon in order to have a uniform criteria for all cases. Laparoscopic resection of endometriosis was performed as previously described (Ávila, 2008; Costa et al., 2010). Segmental recto-sigmoid resection was preformed when bowel function was greatly impaired and when radiological diagnosis of intestinal endometriosis confirmed the presence of intestinal lesions associated with marked restriction of the bowel lumen after colonoscopy. Moreover, deciding the necessity of intestinal resection or intestinal nodule shaving, we took into account endometriosis and intestinal symptoms, impairment of quality of life due to intestinal symptoms, desire of pregnancy and finally the intra-operative evaluation performed by the gynecological surgeon and the coloproctologist. Only after histological confirmation of diagnosis, the patients were included in this analysis. Deep infiltrating endometriosis (DIE) was confirmed when the lesion penetrates >5 mm under the peritoneal surface. We considered intestinal DIE when the lesion infiltrated the muscularis.
RESULTS
During the study period, laparoscopic resection for DIE was carried out in 154 consecutive women. Table 1 presents patient characteristics. Mean patient age was 34.1 years and the majority (n=117;76.9%) were classified as ASRM (1996) stage IV. Most women (n=69; 45%) were infertile although 31% had not attempted to get pregnant at all. Dysmenorrhea was the most frequent symptom (79.3%) followed by chronic pelvic pain (59.7%) and deep dyspareunia (48.7%). Data analysis showed that 14 (9.59%) patients developed postoperative complications. Laparoscopic procedures are summarized in table 2.
Major complications included blood transfusion (n=2) rectosigmoid anastomosis dehiscence (1), rectovaginal fistula (n=1), urinary fistula (n=1), deep vein thrombosis (n=1), lower limb compartment syndrome with motor deficit (n=1) and one intestinal obstruction (n=1). Minor complications were abdominal wall infection (n=3), peripheral neuropathy (n=3), bladder atony (n=1) and bladder perforation (n=1). No deaths were observed. All major complication cases underwent retosigmoidectomy associated with vaginal resection (n=6), uterosacral ligament excision (n=5) or hysterectomy (n=3).
Table 1. Patient characteristics
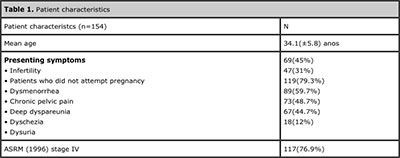
Table 2. Laparoscopic procedures

DISCUSSION
We report the results of 154 surgeries for DIE performed by our multidisciplinary surgical team which is composed of three gynecological surgeons, one coloproctologist and an urologist as well as reproductive endocrinology and infertility specialist. Surgical management of severe disease often requires a multidisciplinary team approach, because surgery may be complex, requiring input from colorectal and urologic colleagues. In our center we have been practicing complete surgical excision of all affected tissue for more than a decade. Our current multidisciplinary approach to surgery was completely established by the beginning of 2000. Laparoscopic skills of the gynecologists, colorectal surgeons, and urologists involved in the endometriosis team were fully developed by this time. The aim of this study was to examine the short term surgical outcome in this group of patients in terms of the rate of surgical complications.
We decided to include only laparoscopies performed by the same gynecologist (IA) and coloproctologist (LMPC) in order to eliminate possible confounding factors although the other surgeons usually participate actively in all procedures.
The 154 women operated on by our team suffered from pelvic pain from but 45% were also infertile and 31% had not even attempted to get pregnant. They were also young (mean age 34.1 years) so fertility preservation was an important issue for many of them. It is now accepted that effective symptomatic management of DIE requires complete excision of the rectovaginal and intestinal disease (Chopin et al., 2005; Dubernard et al., 2006; Seracchioli et al., 2007; Darai et al., 2011; Stepniewska et al., 2009). Recent published data show that the advancements in laparoscopic surgery have enabled a fertility-sparing approach for this group of patients (Darai et al., 2007; Donnez & Squifflet, 2010; Minelli et al., 2010; Pandis et al., 2010; Douay-Hauser et al., 2011; Wattiez et al., 2013). Thus hysterectomy and removal of both ovaries are not mandatory any more. This fertility-sparing approach is effective in reducing pain and improving quality of life and results in increased fertility rates (Fedele et al., 2004; Dubernard et al., 2006; Leyland et al., 2010; Minelli et al., 2010; Darai et al., 2011).
Most cases required extensive surgery as the majority (n=117; 76.9%) were classified as severe endometriosis (ASRM grade IV). This reflects the establishment of our endometriosis team over the years with increasing numbers of women being referred to us for specialized treatment as well as the reported delay of surgical diagnosis of deep infiltrating endometriosis which is significantly longer for patients with advanced stage IV disease (Matsuzaki et al., 2006). The surgical treatment of deep infiltrative endometriosis is challenging and complex. Currently, the gold standard for patient care is the referral to tertiary centers with a multidisciplinary team including gynecologists, colorectal surgeon and urologist with adequate training in advanced laparoscopic surgery (Simoens et al., 2012). The surgical technique is essential to adequately manage the disease and to minimize the risk of complications. In addition, collaboration between gynecologists, urologists, and colorectal surgeons is of paramount importance for successful management of the case in one surgical intervention providing minor risk of complications, shorter hospital stay, and faster functional recovery (D’Hooghe et al., 2006; Simoens et al., 2012; Dunselman et al., 2014).
Data analysis showed that an overall complication rate of 9.59% and the majority of them could be classified as major complications (n=8; 57.1%). Our rate is compatible with other published studies (Donnez & Squifflet, 2010; Slack et al., 2007; Kondo et al., 2011; De Cicco et al., 2011). Evaluating complications in the surgical treatment of DIE is rather difficult as the majority of the studies are retrospective case series, including only a few women.
De Cicco et al. (2011) published a systematic review on bowel resection in women suffering from endometriosis with 77% of the studies included contained fewer than 50 participants and only four of the 30 studies presented included more than 100 participants. It is not clear from these smaller studies whether the reported cases reflect the complication rate during the surgeons’learning curve. Since the complication rates vary considerably, it is possible that the results are heavily influenced by the current experience of the surgical team (Wright et al., 2011). We do not believe our results are heavily influenced by our learning-curve as most complications developed over the years and were not clustered in the beginning of our work.
Another fundamental point to consider is that our patients were young (mean age 34.1 years) and most (n=69; 45%) were infertile and 31% had not attempted to get pregnant at all. The role of DIE in infertility has not been established so far neither the precise effect of surgery has been defined Somigliana et al., 2009; Pandis et al., 2010; Somigliana et al., 2011). Whereas some consider that conservative surgery for rectovaginal endometriosis in infertile women does not modify the reproductive prognosis although it does increase pain-free survival time while increasing complication rates (Costa et al., 2010; Somigliana et al., 2011). Others, however, state that surgery not only does not affect chances of conception, but results in increased conception rates (Fedele et al., 2004; Donnez & Squifflet, 2010; de Ziegler et al. 2010).
The current evidence strongly supports the effectiveness of radical laparoscopic resection in relieving endometriosis-associated symptoms and enhancing psychological well-being. In addition, studies suggest a general improvement of quality of life, however, further studies are needed to support this observation. It must be noted however that extensive surgery for intraperitoneal and deep endometriosis in infertile women does not modify global fertility outcome but is associated with a higher complication rate (Wattiez et al., 2013). A review (Vercellini et al., 2012) of 11 selected studies, the mean post-operative conception rate in all women seeking pregnancy independently of preoperative fertility status and IVF performance was 39% (223/571), but dropped to 24% (123/510) in infertile patients who sought conception spontaneously.
The 15% difference is statistically significant. Thus infertile women with rectovaginal endometriosis considering surgery, should be carefully informed of the real probability of post-operative conception avoiding generic overestimations.
We have previously published an evaluation of 98 women with intestinal endometriosis in order to identify the types of surgical procedures performed and the operative morbidity in women with bowel endometriosis.
Operative morbidity was observed in 9.2% and major complications were rectovaginal fistula (1%) and anastomosis dehiscence (1%). After a mean follow-up of 14 months that included 42 patients, recurrence of clinical symptoms (pelvic pain and dyspareunia) was observed in 8 cases as well as 4 cases of asymptomatic intestinal wall endometriosis recurrence which was identified by ultrasonography (Costa et al., 2010).
Networks and centres of excellence within a multi-disciplinary context is the only way forward to ensure that women with persistent/chronic endometriosis receive consistent, evidence-based and cost-efficient care within a framework which is able to provide excellence, continuity of care, a multidisciplinary approach, research, training and cost effective management (D’Hooghe et al., 2006; Simoens et al., 2012; Dunselman et al., 2014).
Our findings are in agreement with recent published papers which emphasize that a well-trained multidisciplinary team can perform surgical treatment of DIE laparoscopically with low incidence of major complications (Bachmann et al., 2014) though we report on a much larger case series.
CONCLUSION
DIE affects young women for whom fertility preservation is a major issue. The surgical treatment of DIE is complex and subject to complications. This should be taken into consideration when deciding on treatment.
Laparoscopic excision of deeply infiltrating pelvic endometriosis within a multidisciplinary setup in a tertiary referral center appears to be safe with a low rate of significant short-term complications.
The surgical expertise of a multidisciplinary team to allow for a fertility-sparing approach plays a vital role in this setting since most women we treated were infertile, had ovarian endometriomas and a third had never attempted pregnancy.
Bachmann R, Bachmann C, Lange J, Krämer B, Brucker SY, Wallwiener D, Königsrainer A, Zdichavsky M. Surgical outcome of deep infiltrating colorectal endometriosis in a multidisciplinary setting. Arch Gynecol Obstet. 2014. [Epub ahead of print]
Medline Crossref
Chapron C, Chopin N, Borghese B, Foulot H, Dousset B, Vacher-Lavenu MC, Vieira M, Hasan W, Bricou A. Deeply infiltrating endometriosis: pathogenetic implications of the anatomical distribution. Hum Reprod. 2006;21:1839-45.
Medline Crossref
Chopin N, Vieira M, Borghese B, Foulot H, Dousset B, Coste J, Mignon A, Fauconnier A, Chapron C. Operative management of deeply infiltrating endometriosis: results on pelvic pain symptoms according to a surgical classification. J Minim Invasive Gynecol. 2005;12:106-12.
Medline Crossref
Cornillie FJ, Oosterlynck D, Lauweryns JM, Koninckx PR. Deeply infiltrating pelvic endometriosis: histology and clinical significance. Fertil Steril. 1990;53:978-83.
Medline
Costa LMP, Avila I, Filogonio IDS, Machado LGR, Carneiro MM. [Laparoscopic treatment of 98 women with bowel endometriosis]. Rev Bras Colo-proctol. 2010,30:30-6.
Crossref
Darai E, Ackerman G, Bazot M, Rouzier R, Dubernard G. Laroscopic segmental colorectal resection for endometriosis: limits and complications. Surg Endosc. 2007;21:1572-7.
Medline Crossref
Daraï E, Lesieur B, Dubernard G, Rouzier R, Bazot M, Ballester M. Fertility after colorectal resection for endometriosis: results of a prospective study comparing laparoscopy with open surgery. Fertil Steril. 2011;95:1903-8.
Medline Crossref
De Cicco C, Corona R, Schonman R, Mailova K, Ussia A, Koninckx P. Bowel resection for deep endometriosis: a systematic review. BJOG 2011;118:285–91.
Medline Crossref
D’Hooghe T, Hummelshoj L. Multi-disciplinary centres/networks of excellence for endometriosis management and research: a proposal. Hum Reprod. 2006;21:2743-8.
Medline Crossref
Donnez J, Squifflet J. Complications, pregnancy and recurrence in a prospective series of 500 patients operated on by the shaving technique for deep rectovaginal endometriotic nodules. Hum Reprod. 2010;25:1949-58.
Medline Crossref
Douay-Hauser N, Yazbeck C, Walker F, Luton D, Madelenat P, Koskas M. Infertile women with deep and intraperitoneal endometriosis: comparison of fertility outcome according to the extent of surgery. J Minim Invasive Gynecol. 2011;18:622-8.
Medline Crossref
Dubernard G, Piketty M, Rouzier R, Houry S, Bazot M, Darai E. Quality of life after laparoscopic colorectal resection for endometriosis. Hum Reprod. 2006;21:1243-7.
Medline Crossref
Dunselman GA, Vermeulen N, Becker C, Calhaz-Jorge C, D’Hooghe T, De Bie B, Heikinheimo O, Horne AW, Kiesel L, Nap A, Prentice A, Saridogan E, Soriano D, Nelen W. ESHRE guideline: Management of Women with Endometriosis. Hum Reprod. 2014;29:400-12.
Medline Crossref
Fauconnier A, Chapron C, Dubuisson JB, Vieira M, Dousset B, Bréart G. Relation between pain symptoms and the anatomic location of deep infiltrating endometriosis. Fertil Steril. 2002;78:719-26.
Medline Crossref
Fauconnier A, Chapron C. Endometriosis and pelvic pain: epidemiological evidence of the relationship and implications. Hum Reprod Update. 2005;11:595-606.
Medline Crossref
Fedele L, Bianchi S, Zanconato G, Bettoni G, Gotsch F. Long-term follow-up after conservative surgery for rectovaginal endometriosis. Am J Obstet Gynecol 2004;190:1020–4.
Medline Crossref
Ford J, English J, Miles WA, Giannopoulos T. Pain, quality of life and complications following the radical resection of rectovaginal endometriosis. BJOG 2004;111:353–6.
Medline Crossref
Fritzer N, Tammaa A, Salzer H, Hudelist G. Effects of surgical excision of endometriosis regarding quality of life and psychological well-being: a review. Womens Health (Lond Engl). 2012;8:427-35.
Medline Crossref
Kavallaris A, Chalvatzas N, Hornemann A, Banz C, Diedrich K, Agic A. 94 months follow-up after laparoscopic assisted vaginal resection of septum rectovaginale and rectosigmoid in women with deep infiltrating endometriosis. Arch Gynecol Obstet. 2011;283:1059-64.
Medline Crossref
Kondo W, Bourdel N, Tamburro S, Cavoli D, Jardon K, Rabischong B, Botchorishvili R, Pouly J, Mage G, Canis M. Complications after surgery for deeply infiltrating pelvic endometriosis. BJOG. 2011;118:292-8.
Medline Crossref
Koninckx PR, Meuleman C, Demeyere S, Lesaffre E, Cornillie FJ. Suggestive evidence that pelvic endometriosis is a progressive disease, whereas deeply infiltrating endometriosis is associated with pelvic pain. Fertil Steril. 1991;55:759-65.
Medline
Kovoor E, Nassif J, Miranda-Mendoza I, Baulon E, Wattiez A. Hematometra following laparoscopic resection of retrocervical and rectovaginal endometriosis. Fertil Steril. 2010;93:2074.
Medline Crossref
Leyland N, Casper R, Laberge P, Singh SS; SOGC. Endometriosis: diagnosis and management .J Obstet Gynaecol Can. 2010;32(Suppl 2):S1-32.
Medline
Mabrouk M, Frascà C, Geraci E, Montanari G, Ferrini G, Raimondo D, Alvisi S, Paradisi R, Villa G, Seracchioli R. Combined oral contraceptive therapy in women with posterior deep infiltrating endometriosis. J Minim Invasive Gynecol. 2011;18(4):470-4.
Medline Crossref
Matsuzaki S, Canis M, Pouly JL, Rabischong B, Botchorishvili R, Mage G. Relationship between delay of surgical diagnosis and severity of disease in patients with symptomatic deep infiltrating endometriosis. Fertil Steril. 2006;86:1314-6.
Medline Crossref
Mereu L, Ruffo G, Landi S, Barbieri F, Zaccoletti R, Fiaccavento A, Stepniewska A, Pontrelli G, Minelli L. Laparoscopic treatment of deep endometriosis with segmental colorectal resection: short-term morbidity. J Minim Invasive Gynecol. 200;14:463-9.
Medline Crossref
Meuleman C, Tomassetti C, D’Hooghe TM. Clinical outcome after laparoscopic radical excision of endometriosis and laparoscopic segmental bowel resection. Curr Opin Obstet Gynecol. 2012;24:245-52.
Medline Crossref
Minelli L, Fanfani F, Fagotti A, Ruffo G, Ceccaroni M, Mereu L, Landi S, Pomini P, Scambia G. Laparoscopic colorectal resection for bowel endometriosis: feasibility, complications, and clinical outcome. Arch Surg. 2009;144:234-9.
Medline Crossref
Minelli L, Ceccaroni M, Ruffo G, Bruni F, Pomini P, Pontrelli G, Rolla M, Scioscia M. Laparoscopic conservative surgery for stage IV symptomatic endometriosis: short-term surgical complications. Fertil Steril. 2010;94:1218-22.
Medline Crossref
Pandis GK, Saridogan E, Windsor AC, Gulumser C, Cohen CR, Cutner AS. Short-term outcome of fertility-sparing laparoscopic excision of deeply infiltrating pelvic endometriosis performed in a tertiary referral center. Fertil Steril. 2010;93:39-45.
Medline Crossref
Porpora MG, Koninckx PR, Piazze J, Natili M, Colagrande S, Cosmi EV. Correlation between endometriosis and pelvic pain. J Am Assoc Gynecol Laparosc. 1999;6:429-34.
Medline Crossref
Seracchioli R, Poggioli G, Pierangeli F, Manuzzi L, Gualerzi B, Savelli L, Remorgida V, Mabrouk M, Venturoli S. Surgical outcome and long-term follow up after laparoscopic rectosigmoid resection in women with deep infiltrating endometriosis. BJOG. 2007;114:889-95.
Medline Crossref
Simoens S, Dunselman G, Dirksen C, Hummelshoj L, Bokor A, Brandes I, Brodszky V, Canis M, Colombo GL, DeLeire T, Falcone T, Graham B, Halis G, Horne A, Kanj O, Kjer JJ, Kristensen J, Lebovic D, Mueller M, Vigano P, Wullschleger M, D’Hooghe T. The burden of endometriosis: costs and quality of life of women with endometriosis and treated in referral centres. Hum Reprod. 2012;27:1292-9.
Medline Crossref
Slack A, Child T, Lindsey I, Kennedy S, Cunningham C, Mortensen N, Koninckx P, McVeigh E. Urological and colorectal complications following surgery for rectovaginal endometriosis. BJOG. 2007;114:1278-82.
Medline Crossref
Somigliana E, Daguati R, Vercellini P, Barbara G, Benaglia L, Crosignani PG. The use and effectiveness of in vitro fertilization in women with endometriosis: the surgeon’s perspective. Fertil Steril. 2009;91:1775-9.
Medline Crossref
Somigliana E, Benaglia L, Vigano P, Candiani M, Vercellini P, Fedele L. Surgical measures for endometriosis-related infertility: a plea for research. Placenta. 2011;32 (Suppl 3):S238-42.
Medline Crossref
Stepniewska A, Pomini P, Bruni F, Mereu L, Ruffo G, Ceccaroni M, Scioscia M, Guerriero M, Minelli L. Laparoscopic treatment of bowel endometriosis in infertile women. Hum Reprod. 2009;24:1619-25.
Medline Crossref
Vercellini P, Fedele L, Aimi G, Pietropaolo G, Consonni D, Crosignani PG. Association between endometriosis stage, lesion type, patient characteristics and severity of pelvic pain symptoms: a multivariate analysis of over 1000 patients. Hum Reprod. 2007;22:266-71.
Medline Crossref
Vercellini P, Crosignani PG, Somigliana E, Berlanda N, Barbara G, Fedele L. Medical treatment for rectovaginal endometriosis: what is the evidence? Hum Reprod. 2009; 24:2504-14.
Medline Crossref
Vercellini P, Barbara G, Buggio L, Frattaruolo MP, Somigliana E, Fedele L. Effect of patient selection on estimate of reproductive success after surgery for rectovaginal endometriosis: literature review. Reprod Biomed Online. 2012;24:389-95.
Medline Crossref
Wattiez A, Puga M, Albornoz J, Faller E. Surgical strategy in endometriosis. Best Pract Res Clin Obstet Gynaecol. 2013;27:381-92.
Medline Crossref
Wright J, Ballard K. The surgical management of rectovaginal endometriosis: plus ça change? BJOG 2011;118:274–7.
Medline Crossref
de Ziegler D, Borghese B, Chapron C. Endometriosis and infertility: pathophysiology and management. Lancet. 2010;376:730-8.
Medline Crossref